Translate this page into:
Accuracy of Rotator Cuff Tears and Tendinosis Diagnoses on Shoulder Ultrasound Performed by a Short-experienced Operator

Corresponding Author: Harshad Arvind Vanjare, Department of Radiology, Christian Medical College and Hospital, CMC, Ida Scudder Road, Vellore – 632 004, Tamil Nadu, India. E-mail: harshadcmc2002@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vanjare HA, Panwar J. Accuracy of Rotator Cuff Tears and Tendinosis Diagnoses on Shoulder Ultrasound Performed by a Short-experienced Operator. Am J Sonogr 2018, 1(9) 1-5.
Abstract
Objective
The objective of the study was to assess the accuracy of ultrasound examination for the diagnosis of rotator cuff tear and tendinosis performed by a short experienced operator, compared to magnetic resonance imaging (MRI) results.
Method
A total of 70 subjects suspected to have rotator cuff tear or tendinosis and planned for shoulder MRI were included in the study. Shoulder ultrasound was performed either before or after the MRI scan on the same day. Ultrasound operator had a short experience in performing an ultrasound of the shoulder. Ultrasound findings were correlated to MRI findings.
Results
Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for the diagnosis of tendinosis were 58%, 84%, 63%, 80%, and 75%, respectively, and it was 68%, 91%, 73%, 88%, and 85%, respectively, for the diagnosis of rotator cuff tear.
Conclusions
Sensitivity for diagnosing rotator cuff tear or tendinosis was moderate but had a higher negative predictive value. Thus, the ultrasound operator with a short experience in performing shoulder ultrasound had moderate sensitivity in diagnosing tendinosis or tears; however, could exclude them with confidence.
Keywords
Operator experience
Rotator cuff
Tear
Ultrasound
INTRODUCTION
Rotator cuff tear is a common problem in the general population,[1-4] and it can be associated with significant morbidity.[5] Magnetic resonance imaging (MRI) is a good tool to diagnose rotator cuff tears.[6,7] With the rapid development of ultrasound technology such as 7.5–18 MHz linear array broad-bandwidth transducers, better penetration of the ultrasound beam, and improvement of image resolution; the sensitivity of ultrasound to diagnose rotator cuff tears has improved significantly and has reached nearly to that of MRI.[6,8] However, operator skill is considered important for performing any ultrasound study. Ultrasound operators in studies demonstrating high sensitivity and specificity of ultrasound in diagnosing rotator cuff tears have had long experience in performing shoulder ultrasound; which often has been in years.[9] There is very limited data with respect of shorter ultrasound operator experience in performing shoulder ultrasound. One study showed good sensitivity and specificity in diagnosing rotator cuff tears which increased through the study as the experience of the operator increased.[10] The current study was planned to assess the accuracy of ultrasound operator with shorter experience in performing shoulder ultrasound to diagnose rotator cuff tendinosis or tear.
METHODS
Ultrasound operator
The ultrasound operator was a radiology resident who had completed 2 years training in general radiology. The resident performed shoulder ultrasound on 2 normal subjects and 20 clinical cases with rotator cuff abnormalities. At the same sitting, the contralateral shoulder was also evaluated using ultrasound (most of which were normal). After performing the ultrasound, MRI findings of the subject were reviewed the same day. This was done over 1 month duration.
Selection and description of participants
The study was approved by the Institutional Review Board. All patients suspected to have rotator cuff tear and planned for MRI of the shoulder presenting consecutively to the radiology department were included in the study after informed consent. The shoulder ultrasound was performed just before or immediately after the shoulder MRI scan, and the ultrasound operator was blinded to the MRI scan findings. Patients who refused to participate in the study were excluded from the study. This study was done over 6 months duration.
Technical information
Siemens ACUSON S2000 ultrasound machine with 5–14 MHz range ultrasound transducer was used for performing shoulder ultrasounds. MRI of the shoulder was done in Philips Achieva 3.0T MRI scanner.
Protocol for performing an ultrasound of shoulder:
The study was explained to the subjects who were made to sit on a rotating chair.
Subjects were made to perform routine maneuvers within comfortable limits; such as external and internal rotation of arm and extreme internal rotation of the arm such that the hand extended toward the contralateral shoulder blade.
Sequence of assessment:
First biceps tendon was assessed with elbow at 90° flexion. The forearm was kept in supination.
Subscapularis was assessed with the arm in external rotation and elbow at 90° flexion. The forearm was kept in supination.
Supraspinatus was assessed after keeping the arm in internal rotation such that the hand extended toward the contralateral shoulder blade.
For assessment of infraspinatus, palm of the hand touched the front of the opposite shoulder.
Ultrasound criteria for rotator cuff pathology[11]
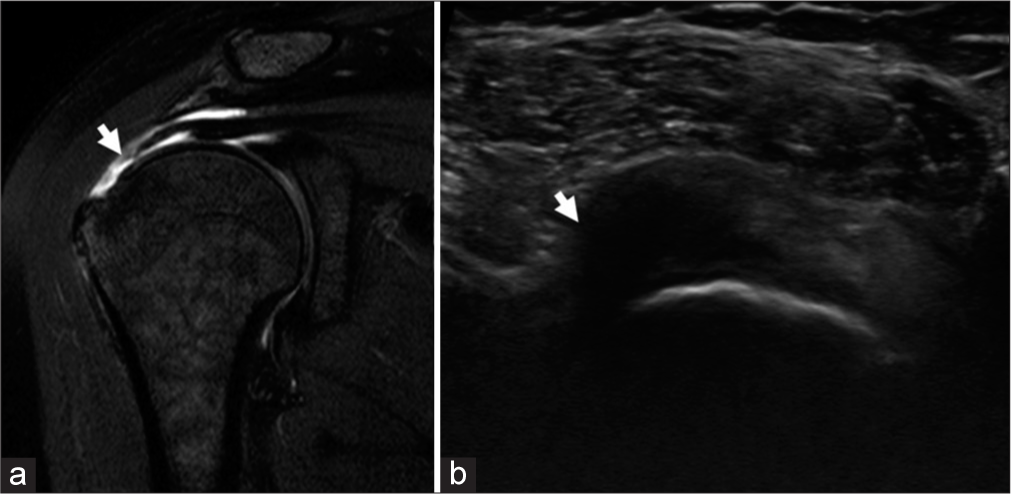
Tendinosis (Figures 1-3)
Characterized by a heterogeneous, ill-defined, and hypoechoic area in the tendon with a variable change in the caliber (enlarged/thinned) without a tendon defect.
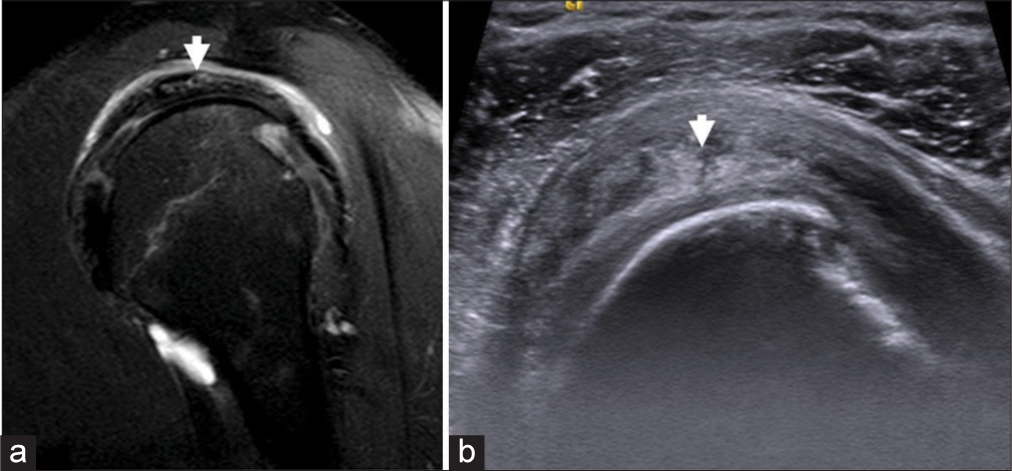
- A 53-year-old male with left shoulder pain, diagnosed to have supraspinatus tendinosis. Image (a) T2 (fat suppressed) sagittal section showing hyperintensity and swelling involving the supraspinatus tendon (arrow). Image (b) Grayscale ultrasound short axis view showing heterogeneous echotexture of the supraspinatus tendon (arrow).
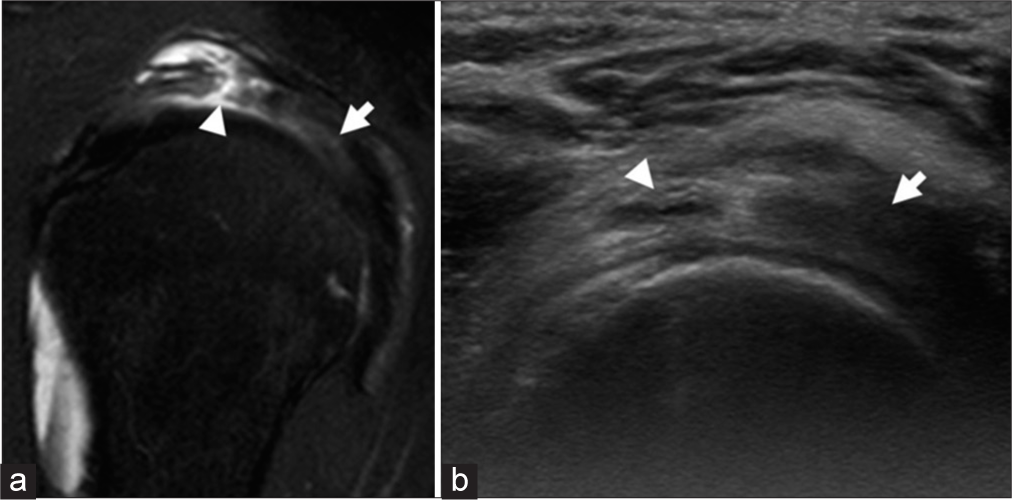
- A 41-year-old male with right shoulder pain, diagnosed to have full thickness tear of supraspinatus tendon with infraspinatus tendinopathy changes. Image (a) T2 (fat suppressed) sagittal section showing focal full-thickness tear (arrowhead) involving supraspinatus tendon with surrounding edema. The infraspinatus tendon (arrow) shows swelling and hyperintensity suggestive of tendinopathy changes. Image (b) Grayscale ultrasound short axis view shows supraspinatus tendon tear (arrowhead) with infraspinatus tendinopathy changes (arrow).

- A 47-year-old male with right shoulder pain, diagnosed to have subscapularis tendinosis. Image (a) T2 (fat suppressed) sagittal section showing swelling and edema involving the subscapularis tendon (arrow). Image (b) Grayscale ultrasound short axis view with bulk and heterogeneous subscapularis tendon (arrow).
Partial thickness tendon tear (Figure 4)

- A 47-year-old male with right shoulder pain, diagnosed to have articular surface partial thickness tear of the right supraspinatus tendon. Image (a) T2 (fat suppressed) sagittal section showing focal area of hyperintensity involving the articular surface of the supraspinatus tendon (arrow) suggestive of a small articular surface tear. Image (b) Grayscale ultrasound short axis view showing corresponding focal hypoechoic area (arrow).
Characterized by a well-defined hypoechoic or anechoic abnormality that disrupt the tendon fibers:
Interstitial tear: Within the tendon substance that does not extend to the bursal or articular surface.
Articular tear: Extends to the articular surface.
Bursal tear: Extends to the bursal surface.
Full thickness tear (Figure 5)
- A 37-year-old female with difficulty in lifting her right arm, diagnosed to have supraspinatus full-thickness tear. Image (a) T2 (fat suppressed) coronal section showing full thickness tear involving the supraspinatus tendon (arrow) at its insertion site with retraction of the tendon. Image (b) Grayscale ultrasound long axis view showing loss of attachment of the supraspinatus tendon to its insertion site with a hypoechoic area extending into the tendon (arrow).
Characterized by a well-defined hypoechoic or anechoic abnormality that disrupts the hyperechoic tendon fibers and extend from the articular to the bursal surface of the tendon.
MRI of the shoulder
The following sequences were acquired in accordance with the institutional protocol:
Proton density weighted (PDW) axial SPAIR (fat suppressed).
T2W SPAIR coronal.
T2W SPAIR sagittal.
PDW coronal.
PDW sagittal.
T1W axial.
MRI scans were reported by two musculoskeletal radiologist with 5 and 10 years of experience.
RESULTS
A total number of subjects included in the study were 70. Fifty-five were men and 15 were women. Average age of the subjects was 39.6 years (±12.6 years). Average age for men was 38.3 years (±12.6 years) and for women it was 44.4 years (±12 years). Right shoulder was evaluated in 45 subjects while left shoulder was evaluated in 25 subjects.
(Table 1) describes true positive and negative and false positive and negative ultrasound studies with respect to MRI.
| Muscle tendons | n | True positive (a) | False positive (b) | False negative (c) | True negative (d) |
|---|---|---|---|---|---|
| Tendinopathy changes | |||||
| Biceps | 67 | 2 | 3 | 6 | 56 |
| Subscapularis | 70 | 11 | 8 | 13 | 38 |
| Supraspinatus | 67 | 35 | 13 | 7 | 12 |
| Infraspinatus | 67 | 4 | 7 | 11 | 45 |
| Tendinopathy changes involving any tendon | 271 | 52 | 31 | 37 | 151 |
| Tear | |||||
| Subscapularis | 70 | 3 | 5 | 10 | 52 |
| Supraspinatus | 67 | 31 | 6 | 4 | 26 |
| Infraspinatus | 70 | 4 | 3 | 4 | 59 |
| Tear involving any tendon | 207 | 38 | 14 | 18 | 137 |
Decimal values in percentages rounded off to the nearest integer. MRI: Magnetic resonance imaging
Subscapularis
Of the 24 subjects diagnosed with tendinosis on MRI, ultrasound detected 11 subjects. Partial thickness tear was diagnosed in 13 subjects on MRI of which ultrasound detected 3 subjects. No subject was diagnosed with complete thickness tear on MRI.
Supraspinatus
Of the 42 subjects diagnosed with tendinosis on MRI, ultrasound detected 35 subjects. 35 subjects were diagnosed to have any tear (both partial and full thickness) on MRI of which 31 were identified on ultrasound. Between complete and partial thickness tear, ultrasound diagnosed 5 of the 12 complete tears and 18 of the 19 partial tears as compared to MRI.
Infraspinatus
Of the 15 subjects with tendinosis, 4 were diagnosed on ultrasound. Four of the 8 subjects were identified with tendon tear on ultrasound as compared to MRI.
Biceps
Of the 8 subjects diagnosed with tendinosis, 2 were diagnosed on ultrasound. No tear was found involving biceps tendon.
DISCUSSION
At present, there is inadequate data with regard to the number of ultrasound required for an operator to be able to diagnose rotator cuff tear with confidence. One study which assessed 2 operators recommended at least 100 shoulder ultrasound before the operators reached a plateau for their skills to diagnose supraspinatus tears.[12] In our study, the ultrasound operator with limited experience in performing shoulder ultrasound (2 normal subjects [4 shoulders] and 20 patients [40 shoulder]) could diagnose rotator cuff tendinosis with sensitivity, specificity, positive predictive value, negative predictive value, and accuracy at 58%, 84%, 63%, 80%, and 75%, respectively, and rotator cuff tear at 68%, 91%, 73%, 88%, and 85%, respectively.
Tendinosis and tendon tears involving subscapularis tendon were repeatedly missed. This may be attributed to normal striated pattern of the tendon[13] and effects of anisotropy, an artifact which occurs when the probe is not held parallel to the tendon. The resulting intra-tendinous hypoechoic appearance may simulate a tendon tear/tendinosis which may be mistaken for pathology. This would cause over or underestimation of actual pathology by an inexperienced ultrasound operator.
The results suggest that although sensitivity and specificity for diagnosing rotator cuff tears and tendinosis for ultrasound operator with limited experience is moderate, except for supraspinatus tendinosis and tears where the sensitivity was moderately good (83% for tendinosis and 89% for tear); the negative predictive values have been good (Tables 2 and 3). This suggests that an inexperienced ultrasound operator can exclude a rotator cuff tear and tendinosis with more confidence than diagnosing them.
| Statistical measures | Absolute values (%) | ||||
|---|---|---|---|---|---|
| Subscapularis | Supraspinatus | Infraspinatus | Biceps | All combined | |
| Sensitivity | 11/24 (46) | 35/42 (83) | 4/15 (27) | 2/8 (25) | 52/89 (58) |
| Specificity | 38/46 (83) | 12/25 (48) | 45/52 (87) | 56/59 (95) | 151/182 (84) |
| Positive predictive value | 11/19 (58) | 35/48 (73) | 4/11 (36) | 2/5 (40) | 52/83 (63) |
| Negative predictive value | 38/51 (75) | 12/19 (63) | 45/56 (80) | 56/62 (90) | 151/188 (80) |
| Accuracy | 49/70 (70) | 47/67 (70) | 49/67 (73) | 58/67 (87) | 203/271 (75) |
Decimal values in percentages rounded off to the nearest integer. MRI: Magnetic resonance imaging
| Statistical measures | Absolute values (%) | |||
|---|---|---|---|---|
| Subscapularis | Supraspinatus | Infraspinatus | All combined | |
| Sensitivity | 3/13 (23) | 31/35 (89) | 4/8 (50) | 38/56 (68) |
| Specificity | 52/57 (91) | 26/32 (81) | 59/62 (95) | 137/151 (91) |
| Positive predictive value | 3/8 (38) | 31/37 (84) | 4/7 (57) | 38/52 (73) |
| Negative predictive value | 52/62 (84) | 26/30 (87) | 59/63 (94) | 137/155 (88) |
| Accuracy | 55/70 (79) | 57/67 (85) | 63/70 (90) | 175/207 (85) |
Decimal values in percentages rounded off to the nearest integer. MRI: Magnetic resonance imaging
The subject selection has been a confounding factor in this study. All the subjects enrolled in the study had high pretest probability for rotator cuff tears or tendinosis (this confounding factor is present in most of the investigations used in a hospital setup). Thus, the estimates for sensitivity and positive predictive values may be falsely raised. If the same operator was to perform shoulder ultrasound in general population with lower pretest probability the sensitivity of the test may be lower. However, in such a case the negative predictive values would be higher than estimated by this study.
Thus, the final conclusion of the study would remain unchanged that an ultrasound operator with limited experience in performing shoulder ultrasound can exclude rotator cuff tear or tendinosis more confidently than diagnosing them.
Limitations
This study is limited by a single ultrasound operator which gives us no idea how multiple ultrasound operators with limited experience would perform in diagnosing rotator cuff tendinosis or tear.
ACKNOWLEDGMENT
This study was done as part of the radiology residency training program (MD in Radiology), and the institution is affiliated to Dr. MGR Medical University, Tamil Nadu, India.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116-20.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of and risk factors for asymptomatic rotator cuff tears in postmenopausal women. Menopause. 2014;21:275-80.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of rotator cuff tear in paraplegic patients compared with controls. J Bone Joint Surg Am. 2010;92:23-30.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of symptomatic rotator cuff ruptures after shoulder trauma: A prospective cohort study. Eur J Emerg Med. 2014;21:349-53.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of rotator cuff tears, including shoulders without pain, on activities of daily living in the general population. J Orthop Sci. 2012;17:136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Detection and measurement of rotator cuff tears with sonography: Analysis of diagnostic errors. AJR Am J Roentgenol. 2005;184:1768-73.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance in the study of the painful shoulder. The surgical comparison in 30 consecutive cases. Radiol Med. 1996;91:348-55.
- [Google Scholar]
- Evaluation of the symptomatic supraspinatus tendon-a comparison of ultrasound and arthroscopy. Radiogr Today. 2002;8:235-40.
- [CrossRef] [Google Scholar]
- Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. 1996. Cochrane Database of Systematic Reviews. John Wiley and Sons, Ltd.; Available from http://wwwonlinelibrary.wiley.com/doi/10.1002/14651858CD009020.pub2/ abstract. [Last cited on 2013 Dec 18]
- [Google Scholar]
- Ultrasound detection of rotator cuff tears: Observer agreement related to increasing experience. AJR Am J Roentgenol. 2010;195:W440-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fundamentals of Musculoskeletal Ultrasound (2nd ed.). Philadelphia, PA: Elsevier; 2013. p. :48.
- Longitudinal analysis of effects of operator experience on accuracy for ultrasound detection of supraspinatus tears. J Shoulder Elbow Surg. 2013;22:375-80.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. 2016;40:975-9.
- [CrossRef] [PubMed] [Google Scholar]







