Translate this page into:
Cord Hemangioma Complicated by Umbilical Vein Rupture; What We Missed on Color Doppler

Corresponding Author: Anne Kennedy, Department of Radiology and Imaging Sciences, University of Utah Hospital, 30 North 1900 East, Room #1A71, Salt Lake City, UT, 84132, United States. E-mail: anne.kennedy@hsc.utah.edu
-
Received: ,
Accepted: ,
How to cite this article: Goldooz M, Draper M, Comstock J, Kennedy A. Cord Hemangioma Complicated by Umbilical Vein Rupture; What We Missed on Color Doppler. Am J Sonogr 2018, 1(10) 1-3.
Abstract
Umbilical cord hemangiomas are rare tumors of the umbilical cord. Doppler ultrasound has been shown to be useful in the diagnosis of cord hemangioma and evaluation of arterial blood flow through the mass. In this study, we present a 28-year-old pregnant woman with an umbilical cord mass with solid and cystic components. She was followed with weekly umbilical artery (UA) Doppler ultrasound, but the fact that the umbilical vein (UV) ran in the wall of the mass was not noted prospectively. At the time of placental delivery, the cystic component of the mass ruptured tearing the UV causing significant bleeding. The case illustrates the importance of using Doppler ultrasound to both look for UA compromise and to map the UV location through the entirety of the cord.
Keywords
Doppler ultrasound
Fetal hemorrhage
Umbilical artery
Umbilical cord hemangioma
Umbilical vein
INTRODUCTION
Umbilical cord hemangiomas are rare tumors of the umbilical cord. Few cases have been reported, and although there may be adverse outcomes, including fetal hemorrhage and death, the clinical significance remains unclear.[1] In this report, we highlight the importance of mapping the umbilical vessels in umbilical cord hemangiomas using Doppler ultrasound.
CASE REPORT
A 28-year-old G3P1102 presented for a screening ultrasound at 23 weeks of gestation. The ultrasound revealed a part cystic, part solid umbilical cord mass arising at the placental cord insertion site in an otherwise healthy fetus with a normal abdominal cord insertion. Doppler ultrasound showed good flow in the umbilical arteries (UAs) which coursed through and around the components of the mass (Figure 1).
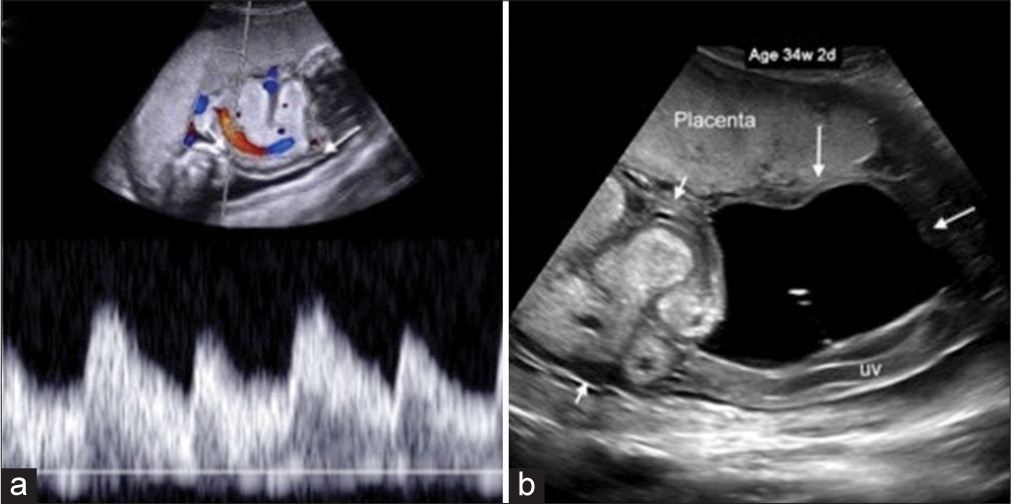
- 28-year-old pregnant woman with umbilical cord hemangioma as an incidental finding on screening ultrasound. (a) Spectral Doppler ultrasound at 33 weeks shows the umbilical artery (UA) coursing through the solid mass. In retrospect, the umbilical vein (UV) (arrow) is visible in the wall of the mass just outside the confines of the color Doppler box. Variable heights of the UA waveform were seen in association with fetal breathing. (b) Grayscale ultrasound of the cord mass at 34 weeks shows the echogenic solid component (short arrows) and the cystic component (long arrows) with a central echo created by the UA which was suspended within the cystic mass. In retrospect, the UV is visible in the wall of the cystic portion of the mass.
The differential diagnosis of a mass in the umbilical cord is relatively small; cord cysts, vascular anomalies, hemangioma, and teratoma. In this case, there was a cystic component within a larger solid mass and no evidence of an umbilical vein (UV) varix or UA aneurysm; therefore, the differential was between hemangioma and teratoma which is difficult based on imaging alone with final differentiation only possible with pathological analysis of the mass showing tissue from all 3 cell lines in a teratoma.
Statistically, hemangioma is much more common, and the location at the placental insertion site is typical of hemangioma as is the homogenously echogenic texture of the mass component.[2] 4 of 14 reported teratomas were associated with omphalocele[3] and this fetus had a normal cord insertion site. Lack of internal calcification also steered us toward the diagnosis of hemangioma.
Due to the reported association of umbilical cord masses with intrauterine fetal demise (IUFD),[4] the patient was followed with weekly UA Doppler ultrasound; there was never evidence of UA compromise. At 33 weeks, the fetus developed a single, echogenic, dilated bowel loop and mild cardiomegaly without signs of hydrops. By 34 weeks, the mass had grown to 19 cm in maximum dimension with a ∼9 cm solid echogenic component and a ∼10 cm cystic component. Labor was induced at 36 weeks 6 days for maternal indications (cholestasis of pregnancy), and she had an uncomplicated vaginal delivery of a healthy male infant. During placental delivery with minimal cord traction and no fundal pressure, the mass ruptured at the vaginal introitus and released a large amount of blood.
Visual inspection of the cord confirmed the large, part-cystic, part-solid mass. The unexpected finding was that the UV ran in the wall of the cystic portion of the mass and tore when the mass ruptured during delivery. The diagnosis of cord hemangioma was confirmed by pathology (Figure 2).

- 28-year-old pregnant woman with umbilical cord hemangioma as an incidental finding on screening ultrasound. (a) Photograph of the fetal surface of the placenta showing the torn umbilical vein (arrow) in the wall of the deflated cystic component of the mass. The solid component is closest to the placental cord insertion. (b) Histology shows a hemangioma characterized by a proliferation of small vascular spaces surrounding the umbilical artery, with capillary-like nodules at the periphery of the lesion (arrowheads).
DISCUSSION
Umbilical cord hemangiomas are rare, and thus, most of the data on outcome is based on case reports or small cohort studies and the clinical significance in any individual case is uncertain. Reported adverse outcomes include fetal hemorrhage and fetal death.
Umbilical cord hemangiomas often consist of two parts: A cystic portion which arises from cystic degeneration of Wharton’s jelly, and a solid portion of angiomatous nodules thought to arise from an umbilical vessel, a vitelline vessel, or the angiogenic mesenchyme of the cord itself.[5]
It is important to differentiate a cord mass from a placental lesion such as a teratoma, thrombosis or hematoma, or an abdominal wall defect such as an omphalocele.[6,7]
Doppler ultrasound has been shown to be useful in the diagnosis of cord hemangioma and evaluation of arterial blood flow through the mass. Fetal hemodynamic compromise has been hypothesized to cause IUFD (36% in one case series) associated with cord hemangiomas.[8] It is important to map arterial flow throughout the cord as flow may appear normal in parts despite the presence of a significant stenosis within the solid tumor.[4] We monitored for potential complications and saw no evidence of umbilical arterial compromise and no progressive signs of a high output state in the fetus. However, although we saw all three vessels running through both the cystic and solid portions of the mass, we did not clearly map the vessels and failed to note prospectively that the UV ran in the wall of the cystic portion of the mass.
During placental delivery, the cystic portion ruptured with associated UV tear; had this happened earlier in labor, it could have led to fetal exsanguination akin to that seen with vasa previa rupture. There are reports of hemorrhage from umbilical hemangioma, resulting in fetal demise.[9] Had we realized that the vein was in the wall of the mass before delivery, we would have elected for Cesarean section over vaginal birth. This case demonstrates that, in the case of a suspected cord hemangioma, it is important to use Doppler ultrasound to not only look for UA compromise but also to map the UV location through the entirety of the cord.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The association of umbilical cord hemangioma with fetal vascular birthmarks. Prenat Diagn. 2005;25:300-3.
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive imaging review of abnormalities of the umbilical cord. Radiographics. 2014;34:179-96.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal diagnosis of fetal umbilical cord teratoma. Case Rep Perinatal Med. 2014;3:4.
- [CrossRef] [Google Scholar]
- A case of umbilical cord hemangioma: Doppler studies and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2009;144:8-14.
- [CrossRef] [PubMed] [Google Scholar]
- Large umbilical cord hemangioma: Sonographic features with surgical pathologic correlation. J Ultrasound Med. 2006;25:1495-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hemangioma of the umbilical cord mimicking an omphalocele. J Pediatr Surg. 1997;32:810-2.
- [CrossRef] [Google Scholar]
- Hemangioma of the umbilical cord: Report of a case. Pathol Res Pract. 2003;199:51-5.
- [CrossRef] [PubMed] [Google Scholar]
- Ruptured hemangioma of the umbilical cord and intrauterine fetal death, with review data. Pathol Res Pract. 2006;202:537-40.
- [CrossRef] [PubMed] [Google Scholar]







