Translate this page into:
Ruptured Scar Pregnancy Secondary to Ingestion of Misoprostol: A Case Report

Corresponding Author: Musarrat Hasan, Department of Ultrasound, Institute Of Ultrasound Imaging, 3/1, Khayaban e Badban, Phase 5, DHA, Karachi - 75500, Sind, Pakistan. E-mail: hasanmusarrat27@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hasan M, Hasan FM, Zafar T. Ruptured Scar Pregnancy Secondary to Ingestion of Misoprostol: A Case Report. Am J Sonogr 2018, 1(8) 1-3.
Abstract
Scar pregnancy is a rare form of ectopic pregnancy. If not diagnosed early and managed appropriately, it may lead to serious complications such as uterine rupture and hemorrhage. We present a case of a 29-year-old female with a history of prior three cesarean sections who presented to our clinic with abdominal pain. She had taken misoprostol to terminate her 6 weeks pregnancy while being unaware that she had a scar pregnancy. Transvaginal ultrasound revealed a ruptured scar pregnancy with hematoma. Emergency laparotomy was performed and uterus was repaired.
Keywords
Color flow Doppler
Ectopic pregnancy
Misoprostol
Scar pregnancy
Ultrasound
Uterine rupture
INTRODUCTION
A pregnancy implanted on a cesarean scar in the uterus is defined as a scar pregnancy. It is a rare form of ectopic pregnancy.[1] A prevalence of 1:1800 has been estimated by Jurkovic et al. in their local population of women taking part in the early pregnancy assessment.[2] Increase in cesarean deliveries has resulted in an increase in the incidence of scar pregnancy.[3] Early evaluation and diagnosis with gray scale and color flow ultrasound can lead to better treatment outcomes, thereby preventing complications including uterine rupture and hemorrhage.[4] In this case report, we present the sonographic features of a ruptured scar pregnancy with live embryo. The patient had taken misoprostol to terminate her pregnancy resulting in uterine rupture while being unaware of the site of implantation of pregnancy.
CASE REPORT
A 29-year-old female with previous history of three cesarean surgeries had taken misoprostol to terminate her pregnancy as she had missed her six menstrual periods. Now, she presented to our clinic with a complaint of lower abdominal pain.
Before coming to our clinic, she had undergone two ultrasound evaluations to assess her pregnancy status. The first transabdominal ultrasound study at a local imaging center confirmed an enlarged uterus, with a single gestational sac corresponding to 4+ weeks and a complex mass that could represent a uterine fibroid. She was advised a transvaginal ultrasound (TVUS). TVUS revealed a normal sized uterus in which the endometrium was not well seen. A mixed solid cystic mass was seen in the lower part of the uterine cavity measuring 5.2 cm × 5.1 cm. In addition, another cystic mass was seen in the lower abdomen anterior to the uterus measuring 10.9 cm × 3.8 cm.
She was thereafter referred to our clinic. TVUS revealed an enlarged uterus normal endometrial cavity (Figure 1) with a gestational sac in the lower uterine segment anterior wall with a fetal pole and cardiac activity (Figures 2 and 3). Color flow Doppler was performed, which demonstrated prominent peritrophoblastic blood flow around the gestational sac. Gestational sac was seen protruding outside from the anterior uterine wall with an accompanying hematoma measuring about 4.5 cm × 4.5 cm in size. These findings were suggestive of scar pregnancy with a hematoma secondary to the rupture of the scar pregnancy. She underwent an emergency laparotomy (Figure 4) confirming a ruptured scar pregnancy.

- A 29-year-old female with scar pregnancy who presented with complaint of lower abdominal pain. Grayscale transvaginal ultrasound in transverse view demonstrates normal endometrial canal (straight arrow).
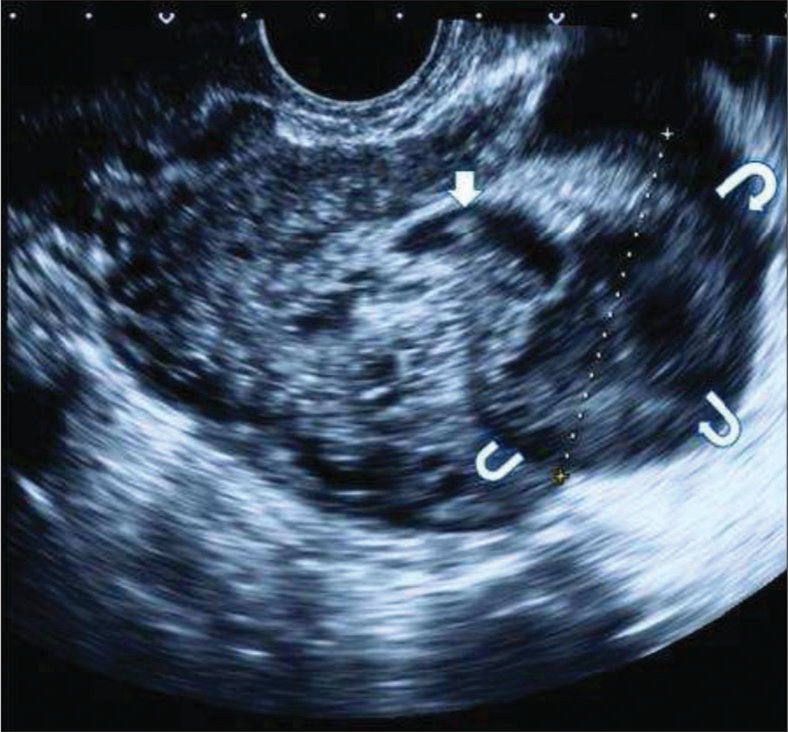
- A 29-year-old female with scar pregnancy who presented with complaint of lower abdominal pain. Grayscale transvaginal sonogram demonstrates a fetal pole (straight arrow) and accompanying hematoma originating from the scar site (curved arrows).
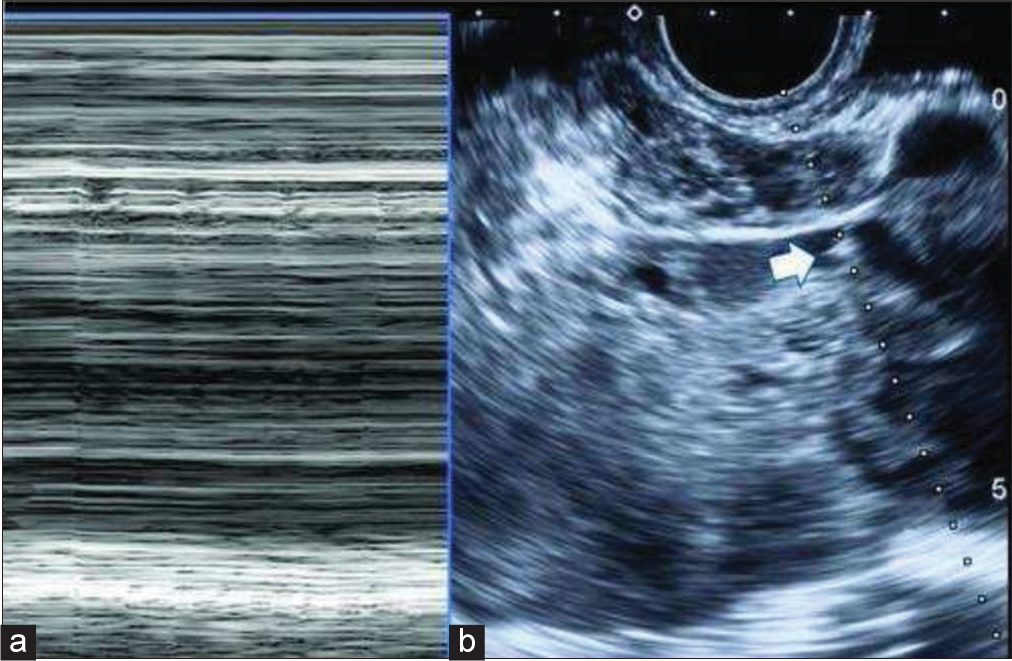
- A 29-year-old female with scar pregnancy who presented with complaint of lower abdominal pain. (a) M-mode demonstrates cardiac activity. (b) Demonstrates fetal pole with M-mode cursor line (arrow).
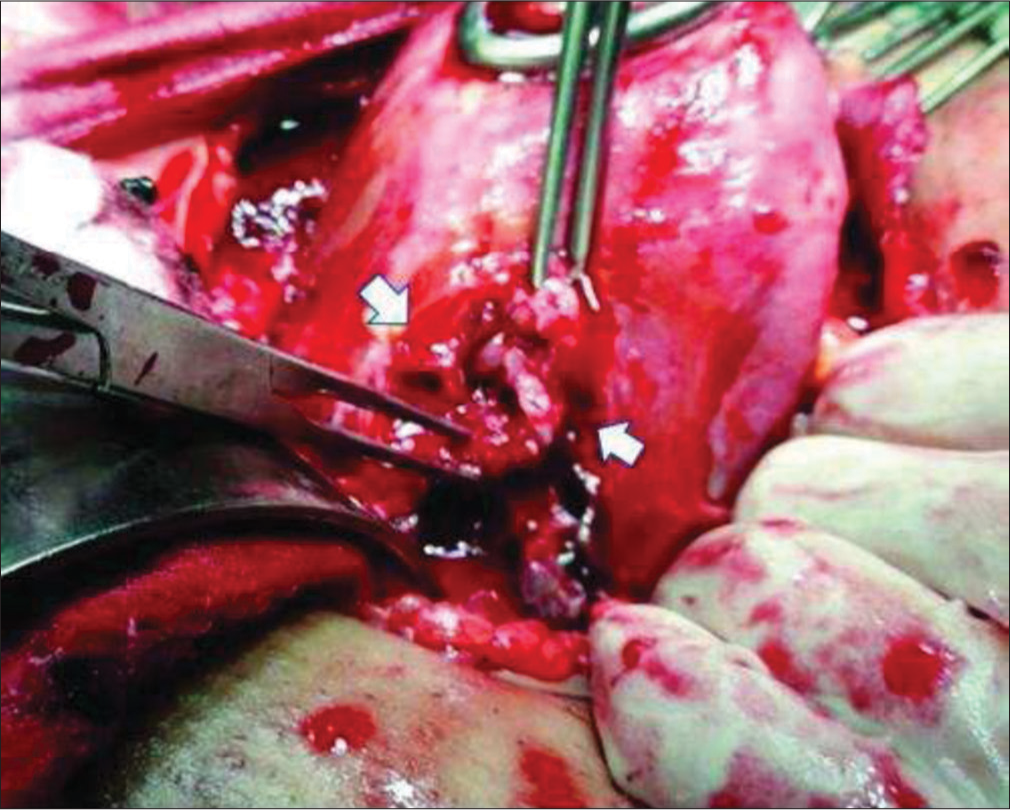
- A 29-year-old female with scar pregnancy who presented with complaint of lower abdominal pain. Laparotomy demonstrates site of rupture (within arrows).
DISCUSSION
Ectopic pregnancy remains the leading cause of death during the first trimester of pregnancy, with a 9%–14% mortality rate. Most patients who have an ectopic pregnancy present with a 5–9 weeks history of amenorrhea, mild pelvic pain, and vaginal spotting.[5]
The main risk factors for ectopic pregnancy include a history of ectopic pregnancy, tubal surgery, and pelvic inflammatory disease and prior cesarean surgeries.[5]
It is important to consider the possibility of a scar pregnancy when risk factors such as previous cesarean section and previous uterine surgeries, dilatation and curettage, myomectomy, and metroplasty are present.[4] In a review of cases of scar pregnancy from 2002 to 2004, Maymon et al. noted that 21 out of 39 (54%) had undergone multiple (≥2) cesareans and 13 had previous dilatation and curettage, which might also be an associated factor.[6]
Furthermore, it has also been noted that cesarean scar pregnancy may have serious complications if not diagnosed early in pregnancy. These include rupture of the uterus at the implantation site and catastrophic hemorrhage.[7] Bladder invasion is a possible sequel if the myometrium is breached completely and the pregnancy is uninterrupted.[7]
Misoprostol, a prostaglandin E1 analog, causes myometrial contractions by interacting with specific receptors on myometrial cells. Adverse effects of misoprostol include uterine hyperstimulation which may lead to uterine rupture. In our case, the patient was advised misoprostol by a local doctor to terminate the pregnancy which is not advisable if the site of pregnancy has not been confirmed by a good quality ultrasound examination. This is because misoprostol appears to increase the risk of rupture of a scar pregnancy.[8] Hence, caution must be exercised when prescribing misoprostol, to avoid complications and preserve future fertility. We recommend that routine ultrasound should be done in early pregnancy before prescribing misoprostol, especially when the patient has had multiple cesarean surgeries in the past.
As was seen in the course of our patient, early abdominal ultrasound examinations did not prove to be of any value in detecting scar pregnancy. TVUS is indispensable in correct diagnosis of scar pregnancy as there is better visualization of the gestational sac and its site of implantation.
It is important to distinguish scar pregnancy from cervical pregnancy. In a cervical pregnancy, the fetus implants in the cervix. In our case, the cervix was differentiated from the scar site by visualizing the spindle-shaped echogenic mucous plug within the cervix. In addition, no myometrium was seen between the gestational sac and the bladder which is very specific of cesarean scar pregnancy.
CONCLUSION
Misoprostol should not be prescribed to the patients for the termination of pregnancy without confirming the exact location of pregnancy. Misoprostol can result in uterine rupture, and the patients with cesarean scar pregnancy are more prone to such rupture.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Musarrat Hasan is on the Editorial Board of the Journal.
References
- Ectopic pregnancy within a caesarean scar: A review. Obstet Gynecol Surv. 2002;57:537-43.
- [CrossRef] [PubMed] [Google Scholar]
- First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 2003;21:220-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cesarean scar pregnancy: Sonographic and magnetic resonance imaging findings, complications, and treatment. J Ultrasound Med. 2012;31:1449-56.
- [CrossRef] [PubMed] [Google Scholar]
- Caesarean scar pregnancy: A diagnosis to consider carefully in patients with risk factors. Ann Acad Med Singapore. 2005;34:216-9.
- [Google Scholar]
- Diagnostic clues to ectopic pregnancy. Radiographics. 2008;28:1661-71.
- [CrossRef] [PubMed] [Google Scholar]
- Ectopic pregnancies in a Caesarean scar: review of the medical approach to an iatrogenic complication. Hum Reprod Update. 2004;10:515-23.
- [CrossRef] [PubMed] [Google Scholar]
- Dilemma in the management of caesarean scar pregnancy. Reprod Syst Sex Disord. 2014;3:125.
- [CrossRef] [Google Scholar]
- Delivery for women with a previous cesarean: Guidelines for clinical practice from the French college of gynecologists and obstetricians (CNGOF) Eur J Obstet Gynecol Reprod Biol. 2013;170:25-32.
- [CrossRef] [PubMed] [Google Scholar]







