Translate this page into:
Glomus Jugulare Tumor Presenting as Deep Vein Thrombosis

Corresponding Author: Maria Zambrano, Touro College of Osteopathic Medicine, Student, Middletown, NY, 10940, United States. E-mail: mzambran2@student.touro.edu
-
Received: ,
Accepted: ,
How to cite this article: Zambrano M, Ko Y, Dogra VS. Glomus Jugulare Tumor Presenting as Deep Vein Thrombosis. Am J Sonogr 2018, 1(11) 1-4.
Abstract
Intraluminal filling defect and non-compressibility of the vein are diagnostic of a deep vein thrombosis (DVT). However, other etiologies can present with features similar to DVTs; these include tumors extending into the vein and primary tumors arising from the vein such as leiomyosarcoma and hemangioendothelioma. Here, we present a case of an 80-year-old female with a right glomus jugulare tumor (GJT) with extension into the right internal jugular vein mimicking a DVT. This case report presents the sonographic features of GJT presenting as DVT and review of the literature of other tumors that can present in a similar fashion.
Keywords
Glomus jugulare tumor
Internal jugular vein
Paraganglioma
Tumor thrombus
Upper extremity deep venous thrombosis
INTRODUCTION
Upper extremity deep vein thrombosis (UEDVT) is a rare clinical finding occurring only in 10–20% of all cases of DVT.[1,2] UEDVT is not only rare but also presents with significant risk as it may result in pulmonary embolism (PE) in one-third of the patients with UEDVT.[1] Among the upper extremity veins, the incidence of thrombosis is approximately 4–30%, higher in the subclavian veins, followed by axillary veins and brachial veins.[1,3] In addition, a higher incidence was found in the left-sided veins at 52.8% than the right-sided veins at 27.6%, according to one retrospective study.[1,4]
In this case report, we present the case of an 80-year-old female who was diagnosed with a possible right internal jugular UEDVT, which was later identified as a right glomus jugulare tumor (GJT).
CASE REPORT
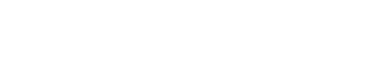
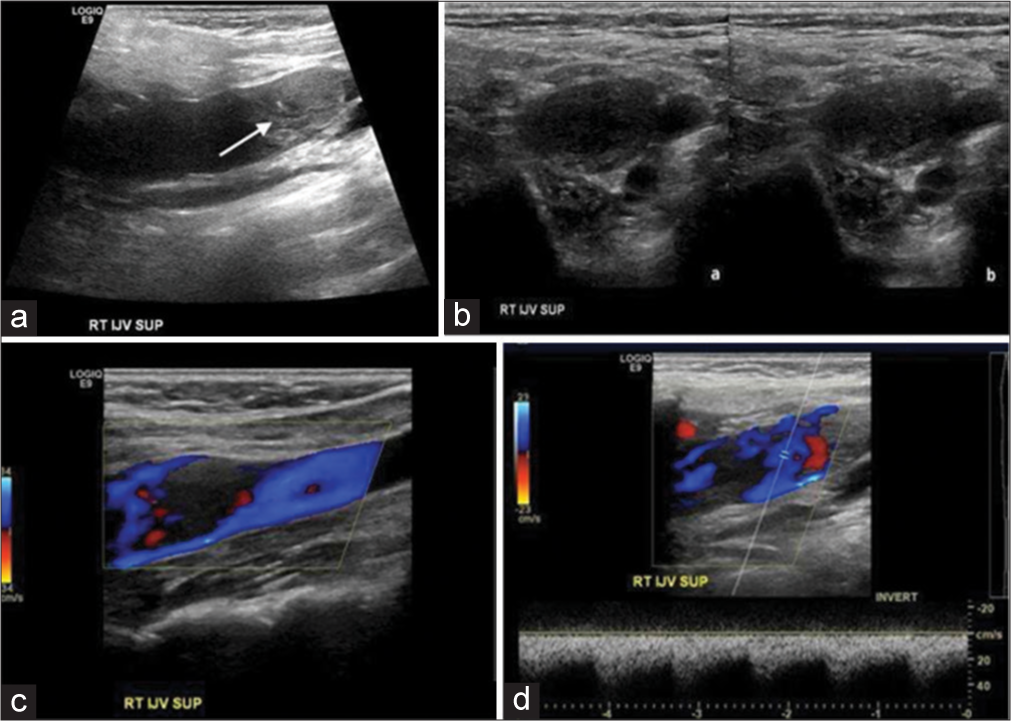
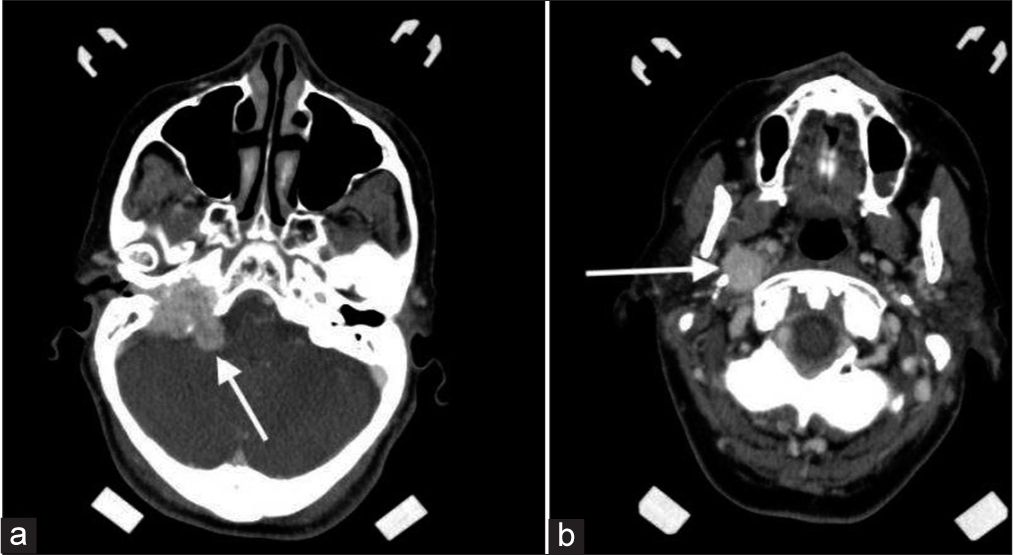
An 80-year-old female presented with progressive symptoms of hearing loss on the right side, tinnitus, symptoms of vocal cord paresis, facial droop, and tongue atrophy. Her medical history includes a presumed arteriovenous fistula found in 1992. There was no significant medical history of the right internal jugular vein (IJV) catheterization. The right upper extremity venous Doppler ultrasound was ordered to exclude a UEDVT. UEDVT revealed an intraluminal filling defect in the right IJV (Figures 1a and b). Color flow Doppler (Figure 1c) was also performed and confirmed the presence of intraluminal filling defect. This was initially thought to be a DVT, but a spectral Doppler of the intraluminal defect revealed the presence of a tumoral blood flow pattern (Figure 1d). Due to the tumoral flow, differential diagnosis of malignant tumor arising from the IJV was considered. Subsequently, the patient underwent computed tomography (CT) and magnetic resonance imaging (MRI) (Figures 2 and 3) and surgery confirming the intraluminal filling defect in the right IJV to be an extension of GJT arising at the right jugular foramen (JF).
- An 80-year-old female with the right glomus jugulare. (a) Gray scale longitudinal ultrasound of the right jugular vein demonstrates intraluminal filling defect and distended internal jugular vein (arrow). (b) gray scale ultrasound image of the right internal jugular vein in transverse plane (a) without and (b) with compression confirming that there is an intraluminal filling defect and vein cannot be compressed. (c) color flow Doppler image of the right internal jugular vein in longitudinal view. Demonstrates intraluminal filling defect. (d) spectral Doppler demonstrates low resistance arterial waveform suggestive of tumor vascularity, thus confirming this to be a malignant thrombus and not a deep venous bland thrombus.
- An 80-year-old female with the right glomus jugulare. (a) Axial contrast-enhanced computed tomography image at the level of cerebellopontine angle demonstrating lesion at the right cerebellopontine angle (arrow). (b) axial contrast-enhanced computed tomography image at the level of upper internal jugular vein demonstrates a contrast-enhancing lesion arising at the right jugular foramen and extending into the right internal jugular vein (arrow). This was surgically confirmed to be a glomus jugulare tumor.
- An 80-year-old female with glomus jugulare. T1 sagittal FLAIR magnetic resonance imaging sequence demonstrates a large mass (arrow) extending from the level of cerebellopontine angle through jugular foramen into the internal jugular vein.
DISCUSSION
The incidence of a UEDVT is about 3/1,000,000 in the general population, making it relatively rare.[2,5-7] UEDVT is classified as primary (non-idiopathic or idiopathic) or secondary in origin as summarized in (Table 1).[6] Primary UEDVT is related to anatomical abnormalities such as thoracic outlet syndrome or Paget-Schroetter syndrome.[2,6-8] If there are no known triggers, it is then classified as idiopathic thrombosis which can be related to malignancy.[8] Secondary UEDVT is related to insertion of central venous catheters at an incidence rate of 14–23%; other sources of secondary UEDVT include arm surgery, trauma, immobilization, and pregnancy.[2,5,6] There is a thrombosis rate of 25–30% of the IJV among all catheter placements; one study showed that IJV catheters have a 4 times greater risk of causing thrombosis than a subclavian catheter.[1,9,10]
| Classification types |
|---|
| Primary |
Non-idiopathic
|
Idiopathic
|
Secondary
|
Another cause of a filling defect in IJV could be a primary leiomyosarcoma of the IJV. Leiomyosarcoma tumors are smooth muscle malignant tumor with higher occurrence in the inferior vena cava but can have intra-abdominal, subcutaneous, and vascular origin.[11,12] Among sarcomas of the head and neck, leiomyosarcomas only make up 4%.[11,13] There are only 41 reported cases of leiomyosarcoma of the head and neck in the English literature.[13]
Another vascular neoplasm is a hemangioendothelioma (HE) tumor, which involves the skin and the superficial or deep soft tissues.[14,15] However, primary vascular HE originating from a large vessel is rare.[14]
In our case, ultrasonography did not identify a gap between the thrombus and the internal jugular foramina. It appeared to be contiguous with the jugular foramina suggesting that it is originating from the jugular foramina or from above that and extending into the IJV. An intraluminal filling defect extending up to the JF raises the possibility that the lesion may be arising from or above the JF. Therefore, primary and secondary lesions that occur at this location should be considered in the differential diagnosis which include intrinsic or extrinsic JF lesion.
If a gap can be demonstrated between the upper end of the IJV thrombus and jugular foramina, it would increase the probability of it being a true UEDVT.
One extrinsic foramen lesion includes chordomas, which are very rare bone tumors arising from remnants of the embryologic notochord.[16] They are most commonly found in the sacrum (50–60%), followed by the clivus and spheno-occipital synchondrosis region (25–30%) which extend laterally to the JF, although it is very rare for a midline lesion to extend laterally to the level of the IJV.[16,17]
Among the intrinsic foramen lesions, paragangliomas (GJT) are the most common and account for 15% of all skull base lesions.[18] GJT is hypervascular tumors which arise within the JF.[19] Paragangliomas arise from glomus cells situated in the adventitia of the jugular bulb. These tumors have the characteristic of following the path of less resistance which include neural foramina and extension into the cerebellopontine or cerebellomedullary angle.[17] GJTs predominantly occur in middle-aged women and most commonly present with tinnitus (76%) and hearing loss (60%), ear fullness, and bruit.[18]
For detecting UEDVT, ultrasound is considered the initial non-invasive imaging test of choice.[2,6,9] Ultrasound scanning includes utilization of two-dimensional scanning with compression testing and color Doppler modes. A systematic review of studies showed high sensitivity of compression ultrasound in diagnosing UEDVT at 56–100% and specificity of 94–100%.[7,9,20] Acute thrombosis includes features such as venous distension, partially compressible or incompressible lumen, hypoechoic, and homogenous appearance of thrombus.[20] An important limitation of ultrasonography is that the clavicle could impair visualization and compression of the subclavian and brachiocephalic veins.[2]
Cross-sectional images are also useful for distinguishing distinct types of thrombi. A bland thrombus can be an isolated thrombus, but it is commonly arising from DVT of the lower extremities. A tumor thrombus is a malignant thrombus representing intraluminal extension versus primary tumor arising from the vein itself. Both MRI and CT have shown to have a higher sensitivity in detecting tumor thrombus and distinguishing it from bland thrombus.[21] Furthermore, tumor thrombus has the presence of enhancement, vessel expansion, and uptake of fluorodeoxyglucose on positron emission tomography.[21,22]
In our case, a spectral Doppler ultrasound was performed, which was helpful in identifying the IJV filling defect as a malignant lesion because of the presence of vascularity within the IJV thrombus. The presence of vascularity in a thrombus differentiates malignant thrombus from a bland thrombus. In addition, we did not identify a gap between the thrombus and the internal jugular foramina suggesting that tumor may be originating at the jugular foramina or from above it. GJTs originate in the skull base and ultrasound cannot penetrate the bone, only giant masses extending inferiorly from the JF to the IJV are possible to detect by ultrasonography.[23] However, the incidence and detection by ultrasonography of a giant GJT are extremely rare with only three individual cases having been recorded in the literature as of February 2018; all previously recorded cases of the GJT included ultrasonographic visualization of a hypoechoic mass elongated into the IJV from the JF, lack of invasion into the venous wall, and rich blood supplies in the mass.[23-25]
MRI and CT play a crucial role in identifying GJTs in addition to the ultrasound findings. In CT, glomus jugular tumors have the appearance of permeative “moth-eaten” pattern representing temporal bone destruction.[17] In MRI, the GJTs give an appearance known as the “salt-and-pepper” pattern on long TR-long TE images which represent signal void and hyperintense foci.[18] The hyperintense foci are due to slow flow and subacute hemorrhage, while the low signal is due to the high flow arterial vessels.[17] MRI has a higher sensitivity in detecting GJT in comparison to CT since it can detect small paragangliomas (<5 mm) as well as involvement of vascular structures such as the internal carotid artery and IJV.[17]
CONCLUSION
Not all intraluminal filling defects in the IJV are DVTs. Other entities, such as GJT as described in this report, can mimic a DVT and should be included in the differential diagnosis. Intraluminal filling defect extending up to the JF and presence of vascularity in the thrombus on spectral Doppler can help in differentiating a mimic versus true DVT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Vikram Dogra is on the Editorial Board of the Journal.
References
- A case of upper left extremity deep vein thrombosis with right side middle lobe syndrome. Ci Ji Yi Xue Za Zhi. 2017;29:180-2.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnostic management of upper extremity deep vein thrombosis: A review of the literature. Thromb Res. 2017;156:54-9.
- [CrossRef] [PubMed] [Google Scholar]
- The arm is not the leg: Pathophysiology, diagnosis, and management of upper extremity deep vein thrombosis. R I Med J (2013). 2017;100:33-6.
- [Google Scholar]
- Incidence of pulmonary embolism and mortality of upper-extremity deep venous thrombosis as compared to lower-extremity deep venous thrombosis in cancer patients. Internet J Pulmonary Med. ;17(1)
- [CrossRef] [Google Scholar]
- Treatment with direct oral anticoagulants in patients with upper extremity deep vein thrombosis. Thrombosis J. 2017;15:26.
- [CrossRef] [PubMed] [Google Scholar]
- Deep Venous Thrombosis (DVT), Upper Extremity. January 2018 Available from: http://www.MEDLINE,Ipswich,MA. [Last accessed on 2018 May 03]
- [Google Scholar]
- Paget-schroetter syndrome with bilateral pulmonary emboli. Radiol Case Rep. 2018;13:28-31.
- [CrossRef] [PubMed] [Google Scholar]
- Upper extremity deep vein thrombosis. Intern Emerg Med. 2010;5:103-9.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombosis associated with right internal jugular central venous catheters: A prospective observational study. Indian J Crit Care Med. 2012;16:17-21.
- [CrossRef] [PubMed] [Google Scholar]
- Central venous catheter-related thrombosis in intensive care patients-Incidence and risk factors: A prospective observational study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2017;161:369-73.
- [CrossRef] [PubMed] [Google Scholar]
- Rare primary leiomyosarcoma of the internal jugular vein with cervical extravascular extension. Br J Oral Maxillofac Surg. 2017;55:192-4.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyosarcoma of the inferior vena cava: Experience in 22 cases. Ann Surg. 2006;244:289-95.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck leiomyosarcoma. Indian J Otolaryngol Head Neck Surg. 2013;65(1):1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelioid hemangioendothelioma arising from interanl jugular vein mimicking cervical metastatic lymphadenopathy. Korean J Thorac Cardiovasc Surg. 2015;48:294-7.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical features of epithelioid hemangioendothelioma in a Han Chinese population: A retrospective analysis. Medicine. 2017;96:e7345.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic factors in skull base chordoma: A systematic literature review and meta-analysis. World Neurosurg. 2018;109:307-27.
- [CrossRef] [PubMed] [Google Scholar]
- Differential diagnosis of jugular foramen lesions. Skull Base. 2009;19:3-16.
- [CrossRef] [PubMed] [Google Scholar]
- Complex glomus jugulare tumor: Management issues. Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl 3):676-81.
- [CrossRef] [PubMed] [Google Scholar]
- Complex tumors of the glomus jugulare: Criteria, treatment, and outcome. J Neurosurg. 2002;97:1356-66.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic and clinical features of upper extremity deep venous thrombosis in critical care patients. Crit Care Res Pract. 2012;2012:489135.
- [CrossRef] [PubMed] [Google Scholar]
- Tumor thrombus: Incidence, imaging, prognosis and treatment. Cardiovasc Diagn Ther. 2017;7(Suppl 3):S165-77.
- [CrossRef] [PubMed] [Google Scholar]
- Role of fluorine-18 fluorodeoxyglucose positron emission tomography in a case of renal cell carcinoma to differentiate tumor thrombus from bland thrombus. Indian J Nucl Med. 2015;30:355-7.
- [CrossRef] [PubMed] [Google Scholar]
- Case report of a rare glomus jugulare tumor extended within the extracranial internal jugular vein: Emphasis on initial ultrasound findings and literature review. Med Ultrason. 2018;20:111-3.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of topography and vascularization of cervical paragangliomas by magnetic resonance imaging and color duplex sonography. Neuroradiology. 2002;44:83-90.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound characteristics of a glomus jugulare tumor. J Neuroimag. 2013;23:242-8.
- [CrossRef] [PubMed] [Google Scholar]