Translate this page into:
Bilateral Testicular Plasmacytomas

-
Received: ,
Accepted: ,
How to cite this article: Croake A, Frances Hall MF, Zhang X, Dogra V. Bilateral Testicular Plasmacytomas. Am J Sonogr 2018, 1(4) 1-4.
Abstract
Intratesticular masses are common and widely presumed to be malignant until proven otherwise. The most common testicular tumors include germ cell and non-germ cell tumors, typically presenting as solitary, unilateral lesions. Some testicular tumors present with bilateral involvement, the most common of which is Leydig cell hyperplasia, with case reports of other synchronous and metachronous bilateral testicular tumors in the literature. Testicular plasmacytomas in the setting of multiple myeloma have been reported as well but are uncommon. Bilateral testicular plasmacytomas are extremely rare. We present sonographic features, with histopathologic correlation in a 71-year-old man who presented with scrotal pain and was found to have bilateral testicular hypoechoic masses confirmed to be plasmacytomas.
Keywords
Color flow Doppler
plasmacytoma
testicular plasmacytoma
testicular tumors
ultrasound
INTRODUCTION
Testicular cancer is the most common solid neoplasm occurring in males between the ages of 20 and 40 and accounts for approximately 1–1.5% of all cancers occurring in men.[1,2] At the time of diagnosis, the majority of testicular tumors are unilateral, with bilateral testicular tumors occurring only 1–2% of the time.[3] Bilateral testicular tumors can occur either metachronously (80–85%) or synchronously (15–20%).[4] We present sonographic features, with histopathologic correlation, in a 71-year-old man who presented with scrotal pain and was found to have bilateral testicular hypoechoic masses confirmed to be plasmacytomas.
CASE REPORT
A 71-year-old man with a past medical history significant for hypertension, hyperlipidemia, benign prostatic hyperplasia, and multiple myeloma was referred by urology for ultrasound examination to evaluate several weeks of vague scrotal pain. Physical examination had been unrevealing.
His multiple myeloma was diagnosed 14 months prior when biopsy of a growing chest wall mass returned as a plasmacytoma. Staging workup otherwise revealed numerous classic lytic skull lesions and a parapineal mass that was also determined to be an intracranial plasmacytoma. Bone marrow aspirate revealed plasma cell myeloma. His treatment regimen included Revlimid, Velcade, and Decadron, and he ultimately underwent autologous stem cell transplantation, resulting in presumed remission.
Ultrasound showed numerous well-circumscribed, somewhat heterogeneous, predominantly hypoechoic masses within the bilateral testicles. These masses showed intralesional vascularity but no intralesional calcifications or fat. The intralesional resistive index was 0.45, suggestive of tumoral flow (Figure 1). A total of two masses were found within the right testis and three smaller masses were discovered on the left (Figure 2). The bilateral testes were otherwise normal in size, with adequate internal arterial and venous vascular flow. The bilateral epididymides were not involved, maintaining their normal sonographic appearance.
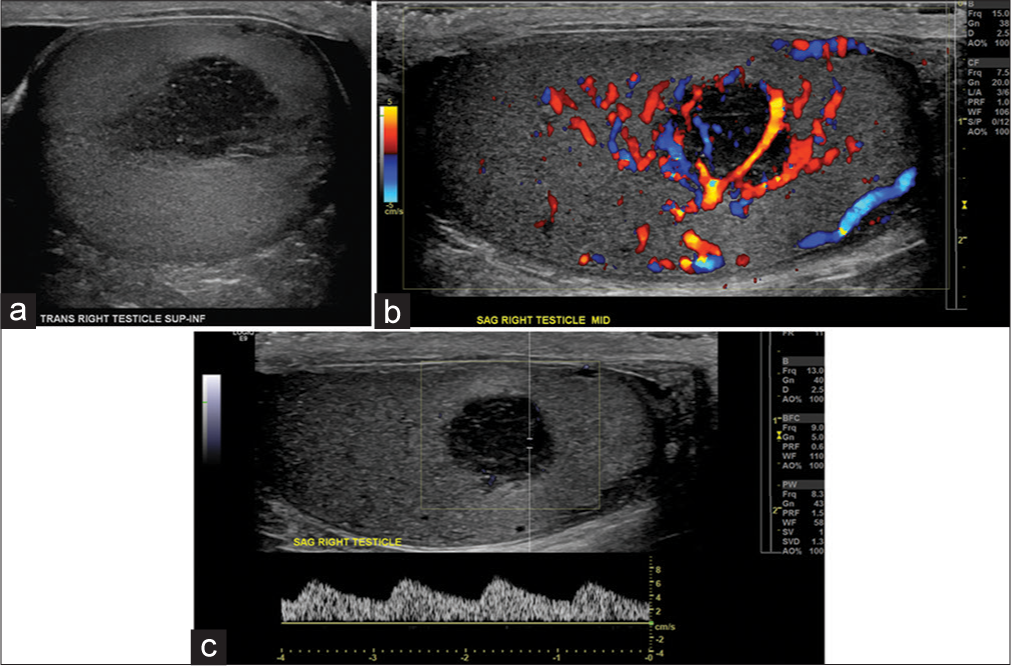
- A 71-year-old man with bilateral testicular plasmacytomas in the setting of multiple myeloma. (a) Grayscale transverse image of the right testis demonstrates a nearly circumscribed hypoechoic lesion within the right testis. (b) Corresponding color flow Doppler imaging demonstrates intralesional vascularity. (c) Spectral Doppler waveform demonstrates tumoral blood flow pattern.
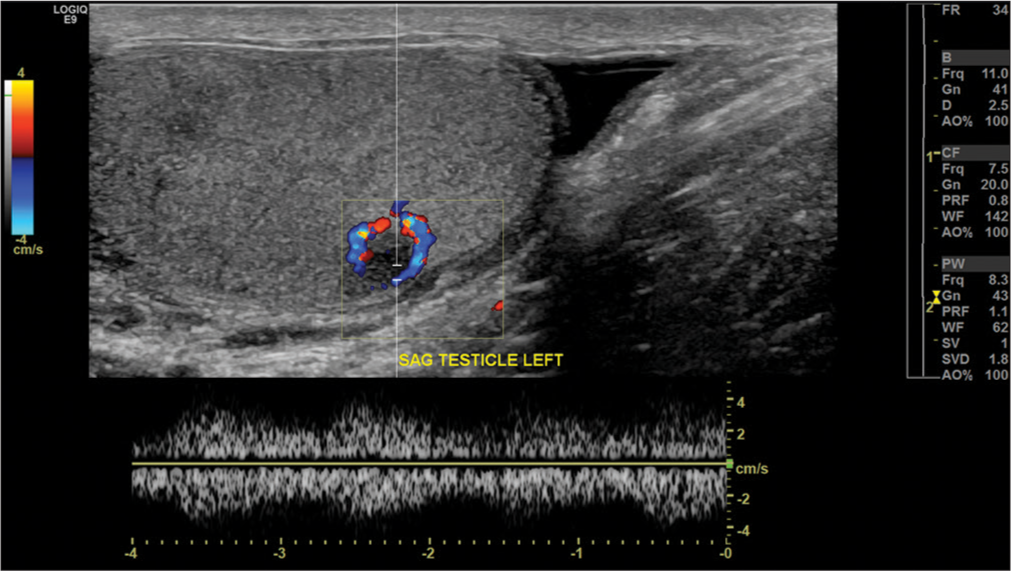
- A 71-year-old man with bilateral testicular plasmacytomas in the setting of multiple myeloma. Color flow Doppler imaging demonstrates a well-circumscribed hypoechoic lesion within the left testis, with intralesional blood flow (only one representative lesion show).
Given these findings, the primary differential diagnosis of Leydig cell hyperplasia or bilateral Leydig cell tumors was proposed; however, in view of the patient’s history of multiple myeloma, the secondary differential of neoplastic testicular involvement from myeloma was also offered. Tumor markers beta-HCG was <1 mIU/mL and alpha-fetoprotein was 3 IU/mL. The patient underwent radical right orchiectomy. He received radiation therapy to the left testis.
Histopathologic sections showed sheets of atypical plasma cells that formed a well-circumscribed mass within the testis parenchyma (Figure 3). The uninvolved background testicular parenchyma showed decreased spermatogenesis. Margins were negative. Concurrent flow cytometry revealed a lambda-restricted plasma cell population positive for CD38, CD138, and CD56. Overall, the picture remained most consistent with plasmacytoma.
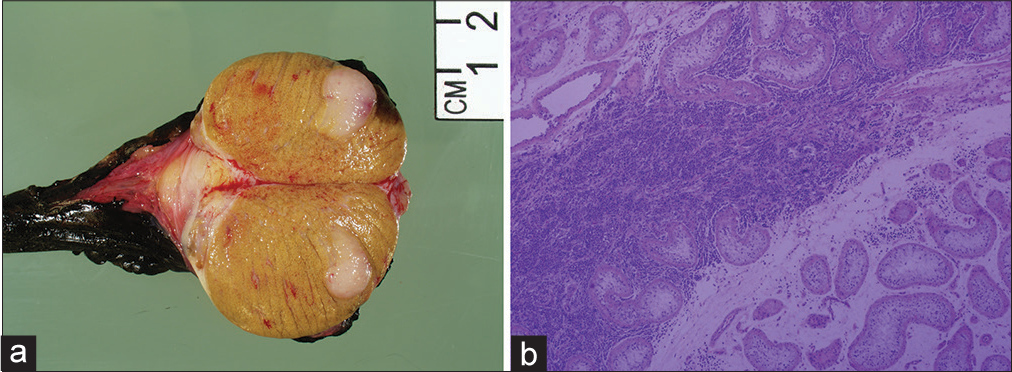
- A 71-year-old man with bilateral testicular plasmacytomas in the setting of multiple myeloma. (a) Gross specimen, showing a well-demarcated 1.5 cm × 1.2 cm × 1 cm tumor which occupies approximately one-fifth of the testicular parenchyma. Tumor does not grossly involve the tunica albuginea or epididymis. The cut surface is tan white and rubbery. (b) Microscopically, tumor shows sheets of atypical plasma cells forming a mass within the testis parenchyma. Numerous mitotic figures are identified including atypical ones. The uninvolved testis shows decreased spermatogenesis. Tumor cells are positive for CD138 while negative for LCA and SALL4, consistent with plasmacytoma.
DISCUSSION
Testicular tumors can be categorized based on their location, intratesticular or extratesticular. Most extratesticular tumors are benign. Frequently encountered tumors include adenomatoid tumors of the epididymis and spermatic cord lipomas, although rarely entities such as rhabdomyomas, lymphomas, sarcomas, cystadenomas, and metastases. Intratesticular masses, the majority of which are malignant, account for 1% of malignancies experienced by men.[1] The most common intratesticular masses are derived from germ cells, of which seminomatous tumors are most often seen. Other common testicular malignancies include non-seminomatous germ cell tumors such as embryonal cell carcinomas, teratomas, and yolk sac tumors. Sex cord-stromal tumors, lymphoma, metastases, plasmacytomas, and leukemic infiltration are also seen but at lower incidences.[1,2,8]
There are several histologic origins of testicular tumors such as germ cell tumors (accounting for 90–95%), sex cord-stromal tumors (approximately 5–10%), and secondary testicular tumors (accounting for <1%).[2] Of these, seminomatous germ cell tumors are the most common giving rise to approximately one-third of all germ cell testicular tumors.[5] The sex cord-stromal tumors come in one of two types: Leydig cell and Sertoli cell tumors, both of which are typically benign. Finally, secondary testicular tumors are defined as tumors that arise in a different organ and then spread to the testes, with lymphoma being the most common.[2]
Rarely, the testis can be a site for other secondary tumors, such as a plasmacytoma (0.03–0.15% of all testicular tumors), which is a solitary mass of neoplastic monoclonal plasma cells.[6] Plasmacytomas can occur in either bone (solitary osseous plasmacytoma) or soft tissues (extramedullary plasmacytoma), the latter of which represents only 3–5% of all plasma cell neoplasms.[3] The testis is a rare site for extramedullary plasmacytoma, which typically occurs in the head and neck region, central nervous system, upper respiratory system, or gastrointestinal system.[7] Most commonly, testicular plasmacytomas present as part of the multiple myeloma disease process or as a site of disease recurrence, but like other testicular tumors, they rarely occur bilaterally and synchronously.[8]
Multiple myeloma is a neoplastic process defined by monoclonal proliferation of plasma cells within the bone marrow. This classically results in osseous insult, although other manifestations include hypercalcemia, anemia, renal insufficiency, and infection.[9] Multiple myeloma exists on the spectrum of plasma cell dyscrasias, which also includes smoldering myeloma, systemic light chain amyloidosis, and Waldenströms macroglobulinemia. Plasmacytomas also fall on this spectrum and can be seen as part of a larger diagnosis of a patient with multiple myeloma or may present as solitary masses. Plasmacytomas can occur in bone, where they are considered solitary osseous plasmacytomas, or in extraosseous tissues throughout the body, where they are called extramedullary plasmacytomas. Extramedullary plasmacytomas are rare and account for 3–5% of plasma cell neoplasms.[3] Occurrence within the testicle is even more rare and makeup <0.2% of all testicular tumors, although it has been estimated that upward of 2% of patients with multiple myeloma will be found to have testicular plasmacytomas at the time of autopsy.[1,3,6] More typically, solitary extramedullary plasmacytomas are seen in the head, neck, respiratory, gastrointestinal, and central nervous systems.[3,7]
While plasmacytomas within the testes in the setting of multiple myeloma are an uncommon but known entity, to have synchronous bilateral lesions is an extremely rare occurrence, with 5 such cases report in the literature. Synchronous cancer can be defined by the presentation of lesions simultaneously or those occurring within 6 months of one another.
Like most testicular malignancies, the typical presentation of a testicular plasmacytoma is as a firm, palpable mass within the testis that may be tender. Such lesions are most commonly found in patients between ages 55 and 60, often with a known diagnosis of multiple myeloma or at the time of known systemic relapse.[8,10,11] Several cases have been reported where these lesions presented in the absence of such history.[3,10] The patient we present here was above average for age and had previously undergone chemotherapy and autologous bone marrow transplantation for treatment of his known myeloma, so the discovery of his bilateral testicular plasmacytomas was thought to be most consistent with disease recurrence.
Sonography is the primary mode of imaging in detection and evaluation of testicular masses and has been shown to have up to 100% sensitivity in their detection.[1] Although our patient presented with only vague scrotal pain, the use of ultrasound was key in this patient’s workup. The typical sonographic appearance, as is demonstrated here, is of a discrete, mostly well-circumscribed mass lesion that is predominantly hypoechoic on grayscale imaging, with robust internal vascularity on color and Doppler flow imaging.[8,12] As with other testicular malignancies, the treatment regimen includes radical orchiectomy, often with concurrent radiotherapy, so accurate and timely recognition of these lesions is crucial.
CONCLUSION
Bilateral synchronous testicular tumors are extremely uncommon. In the presence of multiple, bilateral, hypoechoic, and hypervascular testicular lesions, plasmacytomas should be considered in the differential diagnosis. This is, especially, true in patients with multiple myeloma, even in the absence of palpable abnormality at the time of physical examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Vikram Dogra is on the Editorial Board of the Journal.
References
- Testicular cancer from diagnosis to epigenetic factors. Oncotarget. 2017;8:104654-63.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral synchronous plasmacytoma of the testis. Proc (Bayl Univ Med Cent). 2016;29:196-7.
- [CrossRef] [Google Scholar]
- Synchronous bilateral testicular tumors with different histopathology. Case Rep Urol. 2015;2015:492183.
- [CrossRef] [PubMed] [Google Scholar]
- Testicle, Seminoma. In: Stat Pearls. Treasure Island (FL): Stat Pearls Publishing; 2017.
- [Google Scholar]
- An extramedullary plasmacytoma in the testicle: A case report and review of the literature. Can Urol Assoc J. 2015;9:E240-2.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple myeloma: A clinicopathologic study of 62 consecutively autopsied cases. Medicine (Baltimore). 1980;59:380-92.
- [CrossRef] [Google Scholar]
- National comprehensive cancer network. Multiple myeloma, version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:230-69.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary bilateral testicular plasmacytoma. Case report and review of the literature. Actas Urol Esp. 2008;32:1039-42.
- [CrossRef] [Google Scholar]
- Bilateral synchronous testicular involvement in multiple myeloma. Case report and review of the literature. Tumori. 1997;83:768-71.
- [CrossRef] [PubMed] [Google Scholar]
- Plasmacytoma of the testis in a patient with previous multiple myeloma: Is the testis a sanctuary site? J Clin Oncol. 2010;28:e456-8.
- [CrossRef] [PubMed] [Google Scholar]







