Translate this page into:
Three-dimensional Hysterosalpingo Contrast Sonography with Lignosal as Contrast for Evaluation of Tubal Patency in the Infertile Women – An Observational Cohort Study

Corresponding Author: Chegondi V N Rao, Department of Ultrasound, Shilpa Scan Centre, Near Post Office, Palakollu, Andhra Pradesh, 534260, India. E-mail: chnr42@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Rao CVN, Sindhu C, Kota MK. Three-dimensional Hysterosalpingo Contrast Sonography with Lignosal as Contrast for Evaluation of Tubal Patency in the Infertile Women – An Observational Cohort Study. Am J Sonogr 2019;2(4):1-8.
Abstract
Objectives
The objectives of the study were to evaluate the two-dimensional (2D)/three-dimensional (3D) hysterosalpingo contrast sonography (HyCoSy) using lignosal (a mixture of lignocaine 2% jelly with normal saline) as a contrast agent for assessing fallopian tubal patency in infertile patients.
Materials and Methods
After obtaining the Institutional Review Board permission, a single center prospective study was conducted to evaluate the validity of 3D-HyCoSy with lignosal to assess the patency of fallopian tubes in infertile women. In total 540 infertile patients were recruited for this study. Bilateral fallopian tube patency was confirmed when fallopian tubes were seen as echogenic tubular structures with peritoneal spill under real-time 3D/2D-HyCoSy.
Results
In the first phase of the study, 2D-HyCoSy without 3D acquisition was made in 20 patients (40 tubes). 2D-HyCoSy with lignosal contrast shown tubal patency in 95% and radiographic hysterosalpingography (HSG) resulted in 97.5% tubal patency with 5% inconclusive results by HyCoSy. In the second phase, data from 520 patients showed bilateral tubal patency in 463 patients (89.03%), unilateral tubal occlusion in 49 patients (9.42%), and bilateral tubal occlusion in eight patients (1.53%). No untoward side effects were noticed and reported by the patients during and after the HyCoSy procedure with lignosal.
Conclusions
3D-HyCoSy with lignosal allowed the entire length of the fallopian tubes to be seen as contrast moved through the fallopian tubes to the fimbrial end. A “shower” of contrast around the ovaries is visualized confirming the peritoneal spill. Use of lignosal provides an alternative imaging method for evaluating the tubal patency in infertile patients.
Keywords
Lignocaine
Saline
Tubal patency
Three-dimensional hysterosalpingo contrast sonography
Infertility
INTRODUCTION
Fallopian tube factors are significantly increased and responsible for up to 25%–33% of infertile women and evaluation of tubal patency plays a key role in infertility workup.[1] At present, several tests are available to assess the tubal patency. Although X-ray hysterosalpingography (HSG) and laparoscopic chromopertubation are regarded as gold standard techniques for diagnosing tubal patency, they have several disadvantages. X-ray HSG using oil or water-based contrast has limitations due to severe pain and carries a risk associated with iodine allergy and ionizing radiation. Laparoscopic chromopertubation evaluation with methylene blue involves a patient admission and has some risk associated with anesthesia, surgical morbidity and is also an expensive technique. Another ultrasound guided modality, hysterosalpingo contrast sonography (HyCoSy) using normal saline and air mixed as contrast (saline infusion sonography) allows the visualization of fluid and air bubbles around the ovaries while doing transvaginal ultrasonography and also a cost-effective technique; nevertheless, it is associated with severe pain, vomiting, and syncopal attacks, and problem of nonvisualization of tubes.[2]
Three-dimensional (3D)-HyCoSy using the Echovist (Schering AG, Berlin, Germany) or Sono Vue (Bracco international BV, Amsterdam, Netherlands) as contrast agents for tubal patency is another ultrasound-guided technique, which contains a suspension of micro air bubbles in an aqueous galactose solution.[3,4] Although 3D-HyCoSy is more accurate without many side effects for evaluation of the uterus, ovaries, and tubal occlusion, the method requires expertise in 3D technique and also Echovist and Sono Vue have limited availability due to high cost. Later, a mixture containing hydroxyl methylcellulose and glycerol as contrast (hysterosalpingo-foam sonography [HyFoSy]) was introduced for tubal patency evaluation (ExEm-gel Gynaecologiq BV, Delft, The Netherlands).[5] Although HyFoSy was also reported as an accurate and safe procedure, non-availability and cost make it less attractive in deploying this method in routine sonography for tubal patency testing, especially in low-income countries.
In view of the limitations cited above in the evaluation of tubal patency, there is a high necessity for the development of a new contrast, which is not only as accurate as currently available contrasts but also should be cost-effective, available, and safe. This led us to develop the novel application of lignocaine (a mixture of 2% lignocaine jelly in normal saline, hereafter referred to as lignosal) as a new ultrasound contrast in HyCoSy procedure. The study was planned with the following objectives: (1) To evaluate the feasibility and reliability of two-dimensional (2D)/3D-HyCoSy using lignosal as contrast agent for assessing fallopian tubal patency in comparison with the X-ray HSG and (2) to further study the HyCoSy using lignosal as a routine technique for the evaluation of tubal patency in a large group of infertile female patients in a prospective observational setting.
MATERIALS AND METHODS
Study design
This prospective nonrandomized observational single-center study was performed at Shilpa Scan Center, a referral scan center at Palakollu, Andhra Pradesh state, in rural India. The present study was designed to execute in two phases. The first phase of the study (n: 20) involves the comparison of the diagnostic efficacy of 2D-HyCoSy using lignosal with X-ray HSG for the standardization and feasibility of the technique for tubal patency evaluation. In the second phase of the study (n: 548), primary and secondary infertile women who were a part of infertility evaluation to undergo timed intercourse or intrauterine insemination were studied to evaluate the beneficial effects of the lignosal as contrast media (Figure 1). Pain episodes, adverse reactions, and clinical pregnancy rate were also recorded. The study protocol was approved by the Institutional Review Board. All the patients were informed about the study objectives, and written consent was obtained from every patient before the start of the study. This study was conducted according to the Declaration of Helsinki for medical research, and approved by the local area ethics committee.
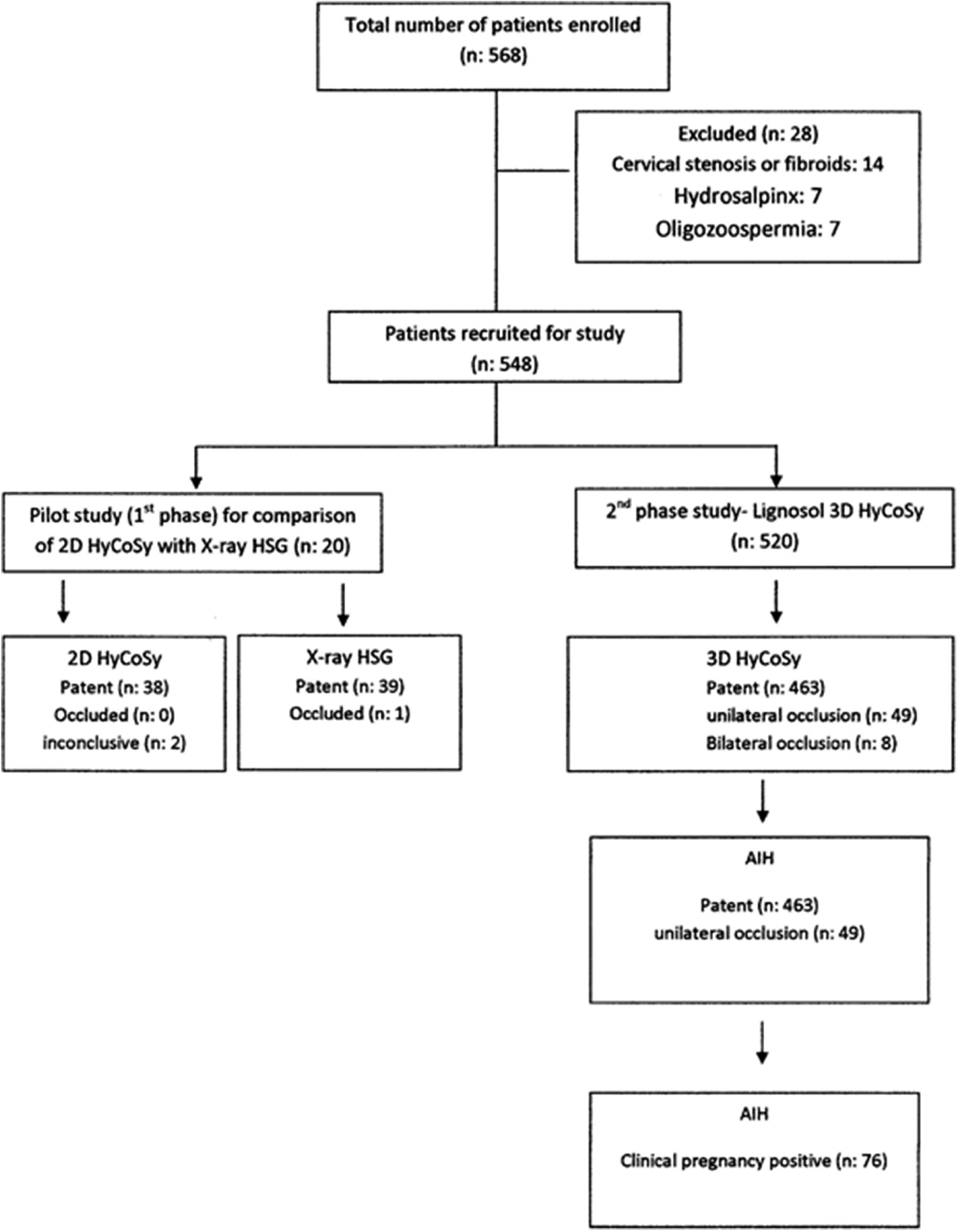
- Flow diagram depicting the plan of the study. (HyCoSy: Hysterosalpingo contrast sonography, HSG: Hysterosalpingography).
Study population
The female infertile patients (n: 568) who referred to our center for sonographic evaluation for the tubal patency test between April 2018 and October 2018 were enrolled in the study. Inclusion criteria for female patients include age <38 years with regular menstrual cycles, normal ovulation and with male partners having a normal semen analysis.[6] Women with pelvic infection, severe pelvic endometriosis, active uterine bleeding, multiple large fibroids, recent surgeries, and non-consent to participate in the trail were excluded from the study. All ultrasound examinations were performed using the Wipro GE Voluson E10 system equipped with 5–9 MHZ and 6–12 MHZ 3D endovaginal probes (GE Healthcare, USA).
Preparation of patients
The procedure involves the administration of 2% lignocaine jelly (Neon Laboratories, India) and normal saline (with a final concentration of 0.2% lignocaine after dilution with saline). Then, the tubal patency procedure is explained to all patients orally, and written consent is taken in the format in advance. A lignocaine test dose is administered to all patients. Injection diclofenac intramuscular 2 ml is given to all patients for the relief of post-procedural pain. A routine transvaginal scan is done to rule out any pregnancy, pelvic infection, uterine, and ovarian pathology. The 3D volume acquisition of uterus and ovaries is done to rule out any uterine malformations and intracavitary lesions. The procedure is done in a lithotomy position while taking strict aseptic precautions. The cervix, vagina, and perineum are cleaned with betadine, perineum draped, and Cusco’s bivalve speculum inserted into the vagina to expose the cervix and fixed with vulsellum if needed. 8F foleys catheter (Romsons, Noida, India) with Steel Stylet is inserted through the cervical canal into the lower endometrial cavity. The bulb is placed just above internal os and is inflated with 0.5–1 ml of water. The stylet is removed and speculum has taken out. Transvaginal probe is introduced and confirmed the position of the bulb.
Preparation of contrast
Lignosal contrast is prepared immediately after the catheter is placed in the uterine cavity. 20 ml of normal saline is taken into 50 cc catheter tip syringe, and 2 ml of lignocaine 2% jelly (20 mg/ml) is taken into 10 cc syringe. The nozzle of 10 cc syringe with lignocaine is connected and fixed to the nozzle of 50 cc syringe containing saline. By agitating the two contents vigorously with to and fro movements between both syringes, a whitish homogenous mixture of microbubbles is formed. The viscosity of contrast is low enough to enable easy passage through the lumen of narrow fallopian tubes, and air bubbles can remain suspended for a longer time of minimum 5–7 mts.
The contrast is slowly injected by a trained nurse into the endometrial cavity through a foleys catheter in repeated small quantities (1–2 ml) while doing transvaginal ultrasonography for observing antegrade flow through the uterine cornua at the transverse plane using B-mode. Fallopian tubes are seen as echogenic, while contrast is flowing through until the fimbrial end where the peritoneal spill is visualized as “shower” around the ovaries.
However, 2D-HyCoSy also has its limitations. In some patients with 2D-HyCoSy fallopian tubes are not seen in a single scanning plane due to its tortuosity. Further, it is difficult to distinguish the fallopian tubes and spill from the surrounding bowels due to echogenic positive contrast medium and due to its similar echogenicity. Combining a 3D ultrasonography with 2D-HyCoSy overcomes these limitations faced with 2D-HyCoSy alone. The automated 3D volume acquisition of the entire fallopian tubes allows easy visualization of contrast medium flow throughout the tubal length and fimbrial ends.
3D-HyCoSy with lignosal
The 3D transvaginal ultrasonography probe is positioned in the vagina, and the uterus is visualized in coronal view and ovaries on either side if possible. 3D volume box was placed over this region and the region of 3D volume acquisition is made as wide as possible so that the uterus, ovaries and the whole length of tubes were visualized. The angles of the 2D scan and 3D volume are set at 180 and 120°, respectively, while the ultrasound contrast is seen flowing into both uterine horns. Volume data acquisition is switched on. Gynec 3D rendering software allowed the volume data of contrast medium in the uterus and fallopian tubes to be obtained automatically for subsequent analysis. The acquisition time of volume is approximately 20 s. Thereafter, the uterus in the coronal section with both tubes on both sides and a view of rings of spilled contrast around the ovaries are visualized. By rotating the volume image, better visualization of tubes in 3D space is possible.
Evaluation criteria for diagnosing tubal patency
2D-HyCoSy
If the tubes are patent, tubes are seen as echogenic while passing contrast agent and spill of contrast from the fimbrial end is seen as “Shower” in the intraperitoneal cavity.
If the tubes are blocked, echogenic tubes and spill are not visualized.
If the tubes are occluded, increased resistance is felt while injecting, due to the backflow of contrast.
In the blocked tubes, strong echogenic star-like spots permeated into myometrium are seen.
3D-HyCoSy
If the tubes are patent, there is no obvious resistance during the injection of contrast medium.
If the tubes are patent, during the 3D acquisition of volume data, steady cord-like echogenic signals of contrast agent through the fallopian tubes from uterine horn are automatically recorded and spill from fimbrial ends also seen.
If the tubes are patent, there is a ring-like spill of microbubbles seen around the ovaries.
If the tubes are occluded, there is an obvious resistance felt while injecting the contrast agent and steady cord like signals is not seen during 3D acquisition. There was no spill of microbubbles seen from fimbrial ends around the ovaries if the ends of the tubes are sac-shaped.
Questionnaire on pain and other side effects
All the patients were asked to report the pain, discomfort and any other side effects during and after 24 h of the procedure. Pain levels were documented as mild, moderate, and severe pain.
Statistical analysis
Descriptive statistics (means, standard deviations, and percentages [%]) were calculated using SPSS, version 21.0 (SPSS Inc, Chicago, USA). Statistical analysis could not be performed between the 2D-HyCoSy with lignosal and X-ray HSG methods in the pilot study due to the small size of the subjects.
RESULTS
Comparison of 2D-HyCoSy with X-ray HSG
A pilot study was carried out to know the concordance between the 2D-HyCoSy with lignosal and the X-ray HSG. During the first phase of the study, 2D-HyCoSy acquisition without 3D rendering was carried out in 20 patients (40 tubes). The findings of all these tests in 20 patients were followed up and compared with X-ray HSG for standardization of HyCoSy procedure with the lignosal contrast medium. All the 38 tubes evaluated by 2D-HyCoSy with lignosal were diagnosed as the patent (a representational video is available showing echogenic tubes on both sides of the ovary while injecting contrast into uterine cavity and spill can be seen from fimbrial ends as a shower and both tubes were patent), whereas HSG diagnosed 39 tubes to be patent out of the total 40 tubes. HyCoSy results were inconclusive in two tubes due to technical problems; however, these were reported to be patent by HSG (Table 1).
| Tubes (n = 40) | 2D lignosal HyCoSy | X-ray HSG |
|---|---|---|
| Patent tubes (number) | 38 | 39 |
| Occluded tubes (number) | 0 | 01 |
| Inconclusive results (number) | 2 | 0 |
| Total | 40 | 40 |
2D: Two-dimensional, HyCoSy: Hysterosalpingo contrast sonography, HSG: Hysterosalpingography
Tubal patency evaluation by 2D- and 3D-HyCoSy
In the 2nd phase of the study, 548 patients were enrolled from April 2018 to October 2018 and 28 patients were excluded for the following reasons. In 14 patients, the catheter could not be introduced due to severe cervical stenosis at either external os or internal os, or due to fibroids at the internal os level. Prior, routine transvaginal ultrasonography detected bilateral moderate hydrosalpinx in seven patients and seven male partners were diagnosed with severe oligozoospermia. Finally, 520 patients were taken for the study of HyCoSy procedure with lignosal to evaluate the feasibility of the method in the large cohort.
Demographic characteristics of patients
The mean average age of the patient was 25.96 ± 4.42 years and the average duration of subfertility was 5.20 ± 3.75 years with the mean body mass index of 21.83 ± 2.10. Out of the total 520 patients, 320 were with primary infertility and 200 patients with secondary infertility which includes 11 patients with unilateral post salpingectomy done for previous ectopic, and 12 patients underwent recanalization, and two patients had ectopic, managed with methotrexate. Out of 520 female patients 65 have small single to multiple fibroids, 34 patients were amenorrheic, 23 patients with adenomyosis, unilateral or bilateral small chocolate cysts were found in 30 patients, unilateral hydrosalpinx in 26 patients, one patient with chronic pelvic kochs, 26 patients with uterine malformations, and 27 patients with ovarian cysts including 14 dermoid cysts were identified. Of the total sample, 280 subjects were from low socioeconomic status (Table 2).
| Parameters | Total (n = 520) |
|---|---|
| Age (years) | 25.96±4.42 |
| BMI | 21.83±2.10 |
| ML (years) | 5.20±3.75 |
| Primary infertility (%) | 320 (61.53) |
| Secondary infertility (%) | 200 (38.46) |
| Female factor | |
| Uterine fibroids (%) | 65 (12.50) |
| Irregular menstruation (%) | 34 (6.53) |
| Adenomyosis (%) | 23 (4.42) |
| Hydrosalpinx (%) | 26 (5) |
| Stenosis (%) | 53 (10.19) |
| PCOS (%) | 55 (10.57) |
| Chocolate cysts (%) | 30 (5.76) |
| Ovarian cysts (%) | 27 (5.19) |
| Uterine malformations (%) | 26 (5) |
| Uterine polyps (%) | 15 (2.88) |
| Tubal patency | |
| Patency (%) | 463 (89.03) |
| Unilateral occlusion (%) | 49 (9.42) |
| Bilateral occlusion (%) | 8 (1.53) |
BMI: Body mass index, 3D: Three-dimensional, HyCoSy: Hysterosalpingo contrast sonography, PCOS: Polycystic ovary syndrome
A combined 2D- and the 3D-Hycosy approach with lignosal contrast medium was followed in 520 patients as a 2D only HyCoSy imaging in 25 out 520 patients failed to see the tubes and spill. Nevertheless, with 3D imaging, tubes, as well as a spill, were seen in 20 out of 25 patients, whereas in 5 patients 3D-HyCoSy failed to detect the pathology and further HSG examination showed bilateral patency in these five patients. Out of total 520 patients, with combined 2D- and 3D-HyCoSy, 463 patients were found with patent tubes, eight patients with the bilateral tubal block and 49 patients with unilateral blocks were diagnosed (Table 2, Figure 2 and Figure 3). Further, 76 patients reported a clinical pregnancy within 2–6 months after the HyCoSy procedure was performed with lignosal.
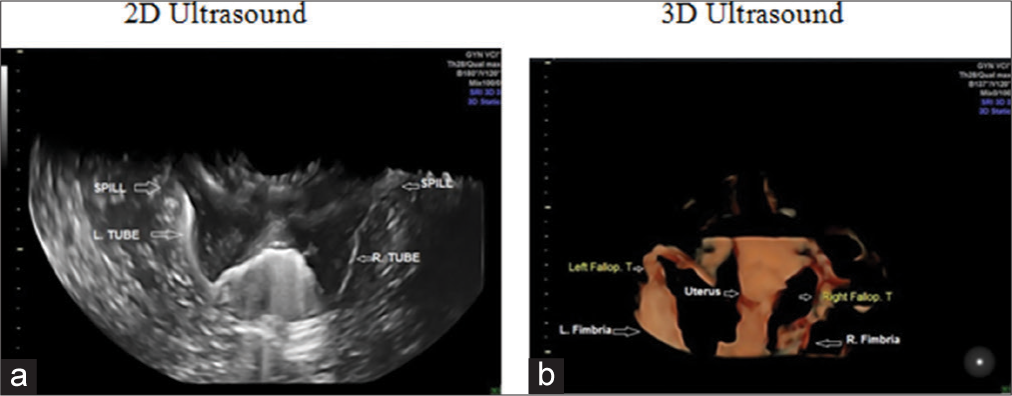
- (a) A 25-year-old women with 6 years of infertility. Two-dimensional hysterosalpingo contrast sonography (HyCoSy) with lignosal contrast showed both tubes as echogenic and spill from fimbrial ends as a shower suggests, bilateral tubal patency. (b) The three-dimensional HyCoSy image of the same patient (25-year-old women with 6 years of infertility) shows both tubes and fimbrial ends.
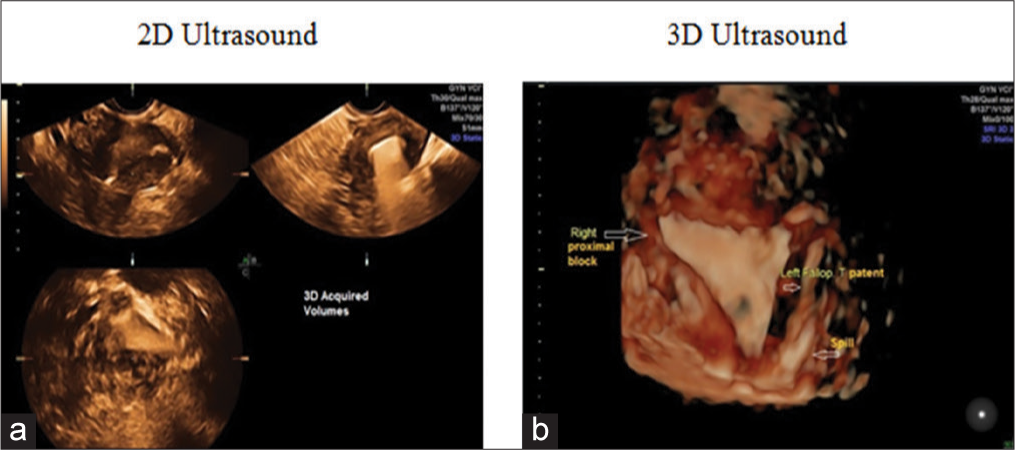
- (a) A 32-year-old lady with 13 years of infertility. H/o right salpingectomy for previous ectopic pregnancy. Two-dimensional hysterosalpingo contrast sonography (HyCoSy) with lignosal shows nonvisualization of both tubes and spill suggests a bilateral proximal block. (b) Three-dimensional HyCoSy of the same patient shows nonvisualization of both tubes (bilateral proximal block).
3D-HyCoSy with lignosal on pain episodes and long-term adverse reactions
All the patients (n: 520) were administered prophylactically with Inj diclofenac, intramuscular, 10 min before the procedure. No patient complained of pain or had a syncopal attack and in no patient HyCoSy procedure was interrupted due to pain episode. A mild-to-moderate procedural discomfort (pelvis) was reported in 240 (46%) women and other side effects with no significance were depicted in Table 3. All the patients were put under observation for possible reactions/complications for a period of 4 months. No untoward side effects were noticed during the above period.
| Event | No. of patients (%) |
|---|---|
| Pelvic discomfort | 240 (46) |
| Syncope | 0 |
| Vaginal bleeding | 47 (9) |
| Fever | 6 (1.15) |
| Headache | 7 (1.34) |
3D: Three-dimensional, HyCoSy: Hysterosalpingo contrast sonography
DISCUSSION
Tubal patency testing constitutes the major part of the tubal infertility management as the tubal disease has a wide spectrum of pathologies, such as obstruction, stenosis, dilatation, and altered peristaltic function, which occurs as a result of changes in the anatomy of fallopian tubes by conditions such as salpingitis, adenomyosis, or any surgical procedures.[7-9] Several of the techniques such as lap-and-dye, though gold standard investigation, do not allow internal assessment of the tube and also carries a risk of morbidity and mortality. HSG considered being a traditional method; however, its application is limited due to iodine allergy and ionizing radiation. With the introduction of HyCoSy, it is now possible to have a real-time assessment of pelvic organs, ovaries, and myometrium. In the present prospective observational setting, we used the 3D-HyCoSy and this is the first of its kind largest study to evaluate the efficacy of lignosal (lignocaine 0.2% jelly with normal saline) as a contrast medium in HyCoSy for testing tubal patency.
Plan to employ 3D-HyCoSy technology in the present study for the evaluation of tubal patency was supported by a previous systematic review which reported a high diagnostic accuracy with 3D-HyCoSy with 98% sensitivity and 90% specificity.[10] 3D volume imaging makes the possibility of complete visualization of entire length fallopian tubes, and this alleviates the false patency results which otherwise may found with the 2D-HyCoSy acquisition in convoluted tubes. In the present study, HyCoSy with lignosal contrast detected tubal patency in 95% of the tubes and radiographic HSG has shown 97.5% tubal patency with 5% inconclusive results by HyCoSy. These results were in agreement with earlier studies where the saline HyCoSy and HSG had similar sensitivity, specificity, and diagnostic predictive values in the diagnosis of tubal patency.[11,12] In the present study, data from 520 patients showed bilateral tubal patency in 463 patients (89.03%), unilateral tubal occlusion in 49 patients (9.42%), and bilateral tubal occlusion in eight patients (1.53%). In one of the earlier studies with HSG, performed as part of routine infertility evaluation in a group of 494 women, the bilateral proximal tubal obstruction was observed in 3% of cases, and unilateral obstruction was seen in 2% of the cases.[13] Data from a total of 272 HSG studies by Bukar et al. revealed a unilateral tubal block in 8.5% of women and the bilateral block in 6.3% women.[14] The variations observed between the present study and previous reports might be due to criteria followed in the intake of subjects during the study settings (age, inclusion, and exclusion of patients with pelvic infections, endometriosis, and fibroids, etc.) and changes in general patient health conditions over time. The concordance rate of 95% observed in the present pilot study between the results of 2D-HyCoSy and HSG. A meta-analysis of three comparative studies of Echovist-200, (solution of galactose and 1% palmitic acid [Echovist-Schering-AG, Germany]) including 1007 women showed that the results of HyCoSy and HSG were identical in 138 of 202 patients (68.3%) or 320 of 384 individual. In our study, a discordant rate of 2.5% (1/40 tubes) was observed between HyCoSy and HSG. The failure of detection of an occluded tube by HyCoSy might not entirely due to the technique as false results can occur with HSG as well as with lap-and-dye, which is not a perfect gold standard and is also susceptible to false occlusion results.[7,15,16]
During the HyCoSy procedure, foleys 8f catheter with steel stylet to facilitate easy insertion of the soft catheter into the uterine cavity was used. Using real-time ultrasound imaging, the passage of echogenic foam through the patent tubes was seen as echogenic from the interstitial portion up to fimbrial ends and spill was visualized as a shower into the peritoneal cavity. In case of the myometrial spasm at the cornual end, the passage of contrast from the interstitial portion was delayed for 2–3 mts. Therefore, in some cases, a waiting period was necessary to visualize the flow. It must be noted that a positive HyCoSy result is conclusive. With the addition of 3D rendering an increased diagnostic accuracy was observed, when compared to only 2D-HyCoSy. If tubal patency cannot be demonstrated, it could be due to the real tubal block or temporary tubal block and due to the myometrial spasm or presence of mucus plugs at the proximal end.
In the first-ever report on gel instillation sonohysterography by Exalto et al., a sterile gel preparation containing hydroxyethyl cellulose, glycerol, lidocaine (2%), and chlorhexidine was used.[17] However, the study did not report the role of the presence of lidocaine (2%) in the gel with regard to echogenicity and study involved direct installation of the gel with intrauterine canula without further dilution. In the present study, we observed a stable microbubble formation (5 min) with a much lower concentration of lignocaine (0.2%) for sonographic examination of tubal patency. Lignocaine, 2% jelly, is already being used as an intrauterine local anesthetic in hysteroscopic procedures, and large quantities of the intraperitoneal lignocaine infusion mixed with saline are being used without any side effects for the relief of pain in post-operative laparoscopic procedures. Lignocaine, 2% jelly, approved by the FDA is a sterile aqueous product which contains methylparaben, propylparaben, hypromellose as preservatives, and available as sterile preparation. Gel also contains sodium hydrochloride to maintain the pH value to 6–7. The effects of lignocaine on fertility were examined in rat mates. The sperm parameters were found to be harmless on either fertility in females or sperm parameters in the male. Gel preparations containing lidocaine and chlorhexidine as an intrauterine, local, and topical anesthetic were used for pain relief during various diagnostic and therapeutic procedures by several authors; however, no demonstrable benefit for the reduction of pain was reported.[18] Since the usage of gel in the present study is limited to small amounts in diluted state (0.2%) in our HyCoSy procedure, no cases of peritoneal irritation were observed and a previous study by Rousseau et al. reported a minimal systemic absorption of lidocaine after the intrauterine administration of lidocaine gel as esthetic even by direct application after endometrial ablation.[19] Moreover, lignocaine gel up to 10% w/w was reported to be safe for vaginal, intrauterine, and intraperitoneal applications.[20] Apart from its central nervous system action properties, lidocaine is also administered as an intravenous infusion for its antiarrhythmic properties. This warrants the heightened attention for systemic safety during the local administration. In a study by Martell et al., the pharmacokinetic data revealed that the peak lidocaine concentration that was observed after a 10% local lidocaine administration for vaginal application was 10–20-fold lower than the concentrations required for the antiarrhythmic regimen.[21] Therefore, with the dose employed in the present study (0.2%) the safety margin is still wider, and there would be of an extremely low chance for systemic toxicity.
Mild pain was reported by some patients and was relieved by administering simple analgesics. No major complications were recorded. No infection was noted in any case. No syncopal attacks were observed. This study illustrates both the feasibility and accuracy of 3D HyCoSy with lignosal contrast (0.2% Lignocaine) in the diagnosis of tubal patency when compared to X-ray HSG. This technique employing lignocaine as contrast was proved to be the most efficient and safe outpatient procedure in present prospective observational study conditions.
Limitations of the study
The limitation with the lignosal contrast is that the echogenic medium might mask intracavitary lesions; however, this can be overcome by application of 3D rendering in which endometrial polyps could be diagnosed accurately. Further large scale prospective randomized multicenter studies are required to confirm the current findings of novel applications of lignocaine and to determine the sensitivity, specificity, and diagnostic accuracy of lignocaine as contrast media when compared with the lap-and-dye method, a gold standard technique in the evaluation of tubal patency.
CONCLUSION
This study illustrates the novel application of lignocaine (0.2%) as a sonography contrast medium. We infer from the present data that the 3D-HyCoSy with lignosal procedure shall be a good alternative when compared to other modalities which are currently available for sonographic evaluation of tubal patency as lignosal contrast found to be a safe, reliable, accurate, and simple outpatient procedure due to ease of accessibility, cost-effectiveness, and moreover may also reduces the pain associated with the procedure.
ACKNOWLEDGMENTS
Authors acknowledge Dr. T L N. Praveen, M.D, R.D, Radiologist, Abhishek scans, Hyderabad, for his suggestions during the preparation of the manuscript. We thank the radiology support team, Mrs. Shilpa, Mr. Madhu, Mrs. Suvarna for technical help. The authors report no conflicts of interest.
References
- Diagnosis of female infertility. A comprehensive approach. J Reprod Med. 1989;34:29-40.
- [CrossRef] [Google Scholar]
- Transvaginal sonographic tubal patency testing using air and saline solution as contrast media in a routine infertility clinic setting. Ultrasound Obstet Gynecol. 1996;7:43-8.
- [CrossRef] [PubMed] [Google Scholar]
- Echovist-200 enhanced hystero-sonography: A new technique in the assessment of infertility. Eur J Obstet Gynecol Reprod Biol. 2005;121:186-90.
- [CrossRef] [PubMed] [Google Scholar]
- Contrast-tuned imaging and second-generation contrast agent SonoVue: A new ultrasound approach to evaluation of tubal patency. J Minim Invasive Gynecol. 2009;16:437-44.
- [CrossRef] [PubMed] [Google Scholar]
- The use of a new gel foam for the evaluation of tubal patency. Gynecol Obstet Invest. 2013;75:152-6.
- [CrossRef] [PubMed] [Google Scholar]
- WHO Laboratory Manual for the Examination and Processing of Human Semen (5th ed.). Switzerland: World Health Organization; 2010.
- Tubal factor infertility, with special regard to chlamydial salpingitis. Curr Opin Infect Dis. 2004;17:49-52.
- [CrossRef] [PubMed] [Google Scholar]
- Adenomyosis and female fertility: A critical review of the evidence. J Obstet Gynaecol. 2012;32:113-6.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional hysterosalpingo-contrast-sonography for the assessment of tubal patency in women with infertility: A Systematic review with meta-analysis. Gynecol Obstet Invest. 2016;81:289-95.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of tubal patency by hysterocontrast sonography (HyCoSy, echovist) and its correlation with laparoscopic findings. J Clin Ultrasound. 1996;24:523-7.
- [CrossRef] [Google Scholar]
- Hysterosalpingo-contrast sonography versus radiographic hysterosalpingography in the evaluation of tubal patency. Int J Gynaecol Obstet. 2009;105:215-7.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of proximal tubal obstruction in patients undergoing infertility evaluation. Acta Radiol. 1994;35:357-60.
- [CrossRef] [PubMed] [Google Scholar]
- Hysterosalpingographic findings in infertile women: A seven year review. Niger J Clin Pract. 2011;14:168-70.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the performance of hysterosalpingo contrast sonography in 500 consecutive, unselected, infertile women. Hum Reprod. 1998;13:1519-26.
- [CrossRef] [PubMed] [Google Scholar]
- Can hysterosalpingo-contrast sonography replace hysterosalpingography in confirming tubal blockage after hysteroscopic sterilization and in the evaluation of the uterus and tubes in infertile patients? Am J Obstet Gynecol. 2011;204:79.e1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Gel instillation sonohysterography: First experience with a new technique. Fertil Steril. 2007;87:152-5.
- [CrossRef] [PubMed] [Google Scholar]
- Topical anesthesia for minor gynecological procedures: A review. Obstet Gynecol Surv. 2002;57:171-8.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma lidocaine concentrations following insertion of 2% lidocaine gel into the uterine cavity after uterine balloon thermal ablation. Br J Anaesth. 2002;89:846-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lignocaine gel in minimally invasive surgery a pilot cohort study. Aust N Z J Obstet Gynaecol. 2010;50:382-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacokinetics of lidocaine and its metabolites following vaginal administration of lidocaine gel to healthy female subjects. Clin Pharmacol Drug Dev. 2017;6:27-35.
- [CrossRef] [PubMed] [Google Scholar]







