Translate this page into:
Transient Hydrocolpos due to Vesicovaginal Reflux

Corresponding Author: Dr. Subramaniyan Ramanathan, Department of Clinical Imaging, Al-Wakra Hospital, Hamad Medical Corporation, PO Box 82228, Doha, Qatar. Department of Radiology, Weill Cornell Medical College, Qatar. Tel.: +974-50117935, Fax: +974-40114509. E-mail: drrmsubbu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramanathan S, Palaniappan Y, Al Heidous M. Transient Hydrocolpos due to Vesicovaginal Reflux. Am J Sonogr 2018; 1(7): 1-3.
Abstract
Hydrocolpos is commonly due to obstructive causes such as imperforate hymen and vaginal septum. Transient hydrocolpos or non-obstructive hydrocolpos is an under-recognized entity due to a phenomenon called “vesicovaginal reflux” (VVR). It is commonly seen during voiding cystourethrography although it is not a familiar entity for radiologists. Failure to recognize VVR often leads to unnecessary higher imaging modalities. We report a case of young married woman who presented with daytime urinary continence and found to have transient hydrocolpos due to VVR.
Keywords
Hydrocolpos
Incontinence
Ultrasound
Vesicovaginal reflux
Voiding urethrogram
INTRODUCTION
Hydrocolpos represents fluid distension of vagina commonly due to imperforate hymen in children and adolescents. It is called hematocolpos when it contains blood products. It can present early in the life as abdominal pain and distension or later as primary amenorrhea.[1] One of the lesser known causes of transient or intermittent hydrocolpos is vesicovaginal reflux (VVR). VVR is defined as reflux of urine into the vaginal vault either in supine or upright position during voiding.[2] The patient presents clinically with various symptoms such as urinary incontinence, recurrent urinary tract infection (UTI), bed wetting, vulvovaginitis, bad smell, and vaginal discharge.[3] Although VVR is a well-known entity among urologists, it is rarely encountered by radiologists leading to diagnostic dilemma. Herein we report a case of transient hydrocolpos due to VVR in a young married women presenting with incontinence.
CASE REPORT
A 27-year-old recently married woman, weighing 65 kg, presented with daytime urinary incontinence for the past few years. Her menstrual history is unremarkable and did not have any surgeries in the past. Physical examination revealed normal external genitalia with signs of mild bacterial vaginitis. On per vaginal examination, no cervical tenderness or palpable mass was felt. Renal function tests and blood counts were within normal limits. Urine examination revealed numerous pus cells, red blood cells, and epithelial cells. There was significant bacteriuria and urine culture showed Escherichia coli growth. Ultrasonography (USG) of the abdomen and pelvis was ordered to rule out any urinary tract anomalies and other pelvic pathologies. USG revealed a large cystic lesion in the midline of the pelvis in close relation to the cervix. The uterus and left ovary were normal, and the right ovary could not be identified. As the radiologist did not expect a hydrocolpos in married girl with normal menstrual history, other possibilities such as adnexal cystic lesion, developmental cysts, and urinary bladder (UB) diverticulum were considered along with hydrocolpos. Routine post-void study showed the complete disappearance of the cystic lesion with partial emptying of the UB. As the on-call radiologist was not aware of this entity, it was initially diagnosed as bladder diverticulum. However, on consultant review, a possibility of hydrocolpos due to VVR was discussed and urologist requested further imaging to rule out any vesicovaginal fistula and ectopic ureteric openings. A computed tomography (CT) urogram was performed which showed normal ureteric openings with no definite bladder diverticulum. Vaginal appears distended with contrast without any demonstrable fistulous communication. Repeat limited low-dose CT of the pelvis showed emptying of vaginal contrast confirming VVR. The patient improved with the treatment of UTI and vaginitis with weight reduction and behavioral therapy (Figures 1 and 2).
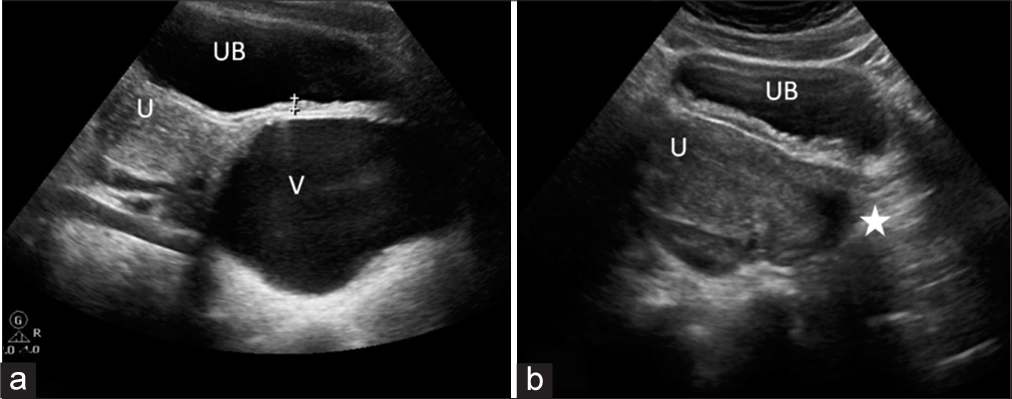
- A 27-year-old woman with a history of urinary incontinence. (a) Ultrasound of the pelvis shows oval cystic lesion inferior to the uterus (U) and posterior to urinary bladder (UB) representing hydrocolpos (V). (b) Post-void ultrasound shows partial emptying of the bladder (UB) with complete disappearance of the cystic lesion (asterisk).
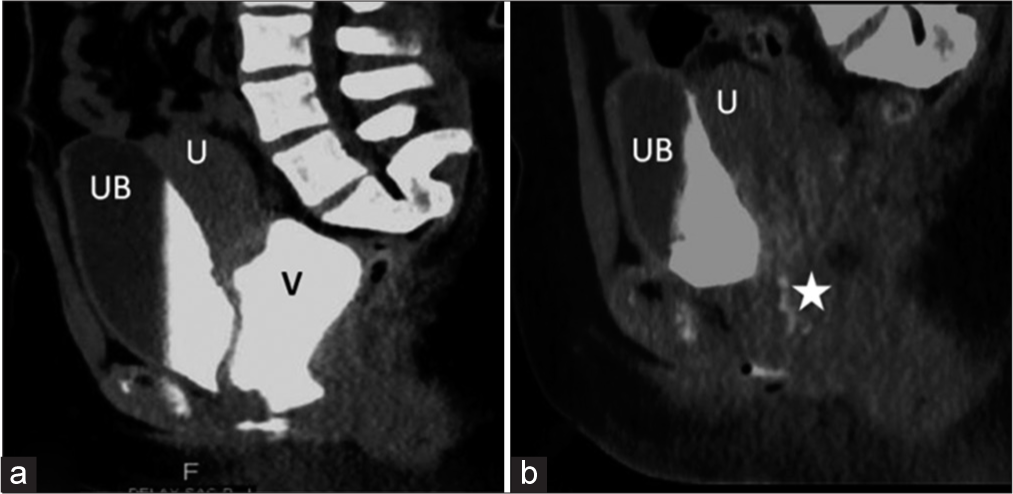
- A 27-year-old woman with a history of urinary incontinence. (a) Sagittal computed tomography (CT) urogram shows contrast filled urinary bladder (UB) and vagina (V) with no definite vesicovaginal fistula. U - Uterus. (b) Post-void CT shows partial emptying of the bladder (UB) with complete disappearance of the cystic lesion (asterisk). U - Uterus.
DISCUSSION
Vesicovaginal reflux (VVR) is a functional voiding disorder seen in prepubertal girls without anatomical or neurological abnormality. Although it is well known to urologists, it may be a diagnostic dilemma for the inexperienced trainee radiologist.[4] It is an underestimated entity reported in 43–69% of girls undergoing imaging evaluation for voiding dysfunction.[5,6] In VVR, there is a reflux of urine from the external urethral meatus into the vagina through the introitus either in supine or erect position. Various etiologies have been proposed: Obesity with tightly opposed, large labia majora which prevent passage of urine, abnormal toileting position, adhesions of labia minora, ureteral duplication or ectopic ureter with insertion into vagina, female hypospadias, and spastic pelvic floor musculature.[3,7,8] Often, it is an incidental finding in pediatric patients undergoing voiding cystourethrogram (VCUG) study. However, it can present in adolescent and adults with recurrent urogenital infections, lower urinary tract symptoms, post-void dribbling, or daytime incontinence.[9] Although VVR is common, hydrocolpos is an infrequent manifestation as there is spontaneous emptying of urine from vagina in erect position, unless there is an associated congenital or acquired vaginal obstructive lesion.
Imaging features
USG is the initial imaging modality in the evaluation of urogenital symptoms and shows pelvic cystic lesion posterior to UB in relation to the uterine cervix in the expected location of the vagina. Although adnexal cystic lesions and bladder diverticulum can mimic these features, close evaluation along with the background knowledge of this entity, it is possible to make a confident diagnosis of hydrocolpos due to VVR.[1,10] Post-void USG is essential to demonstrate the non-obstructive nature of hydrocolpos ruling out imperforate hymen and vaginal septum atresia.
VVR can be diagnosed easily on a VCUG which demonstrates direct filling of the vagina during micturition and resolves on post-void images.[6] Major diagnostic confusion happens when it is seen on pelvic USG.[3,8] Lack of awareness about VVR leads to unnecessary further imaging tests such as CT and magnetic resonance imaging (MRI) like in our patient. However, CT and MRI may be requested by the urologists in symptomatic and non-responding patients to look for associated anomalies such as ectopic ureter and vesicovaginal fistula.[11] Both CT urogram and MRI help in confirming the hydrocolpos and ruling out organic causes. MRI scores over CT due to its better soft tissue resolution and lack of radiation. CT helps in ruling out ectopic ureteric opening better than MRI, whereas MRI is the modality of choice in diagnosing uterovaginal anomalies.[4,10,12]
Treatment is directed at toilet retraining and behavioral therapy to decrease the episodes of VVR.[13] Often, there are underlying urinary and genital infections which need to be treated with appropriate antibiotics. Weight reduction can be helpful in obese patients. VVR is of more interest to radiologist than urologists as it is functional voiding disorder and does not need any specific management. However, it is important for the radiologist to be familiar with this disorder to avoid the chain of exhaustive imaging tests which provokes unwarranted patient and parent anxiety.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Hematometra and hematocolpos: Ultrasound findings. AJR Am J Roentgenol. 1979;132:1010-1.
- [CrossRef] [PubMed] [Google Scholar]
- Vaginal reflux: A forgotten cause of diurnal incontinence in prepubertal girls. Ann Pediatr (Barc). 2015;83:55-6.
- [CrossRef] [Google Scholar]
- Vesicovaginal reflux mimicking obstructive hydrocolpos. J Ultrasound Med. 2007;26:1781-4.
- [CrossRef] [PubMed] [Google Scholar]
- Vesicovaginal reflux: A case report. Indian J Radiol Imaging. 2009;19:235-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vaginal reflux in the miction cystourethrography. Findings in 119 girls (317 per cent) Cesk Pediatr. 1975;30:39-41.
- [Google Scholar]
- The frequency of vaginal reflux during micturition--its possible importance to the interpretation of urine cultures. Pediatrics. 1966;38:293-4.
- [Google Scholar]
- Vesicovaginal reflux: recognition and diagnosis using ultrasound. Pediatr Radiol. 2010;40:114-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nonobstructive hydrocolpos: Sonographic appearance and differential diagnosis. Radiology. 1983;149:273-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nonobstructive hydrocolpos due to vesicovaginal reflux: Expanding the differential diagnosis. Jpn J Radiol. 2015;33:287-90.
- [CrossRef] [PubMed] [Google Scholar]
- Urocolpos due to vesicovaginal reflux. Int Urogynecol J. 2015;26:151-3.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of dysfunctional voiding. Curr Opin Pediatr. 2006;18:139-47.
- [CrossRef] [PubMed] [Google Scholar]







