Translate this page into:
Papillary Cystadenoma of the Epididymis: A Case Report and Review of the Literature

Corresponding Author: Yoon Ko, Touro College of Osteopathic Medicine, 60 Prospect Avenue, Middletown, New York, United States. E-mail: yko@student.touro.edu
-
Received: ,
Accepted: ,
How to cite this article: Ko Y, Nuffer Z, Jean-Gilles J, Dogra V. Papillary Cystadenoma of the Epididymis: A Case Report and Review of the Literature. Am J Sonogr 2018, 1(5) 1-4.
Abstract
We present a case of a 34-year-old male with a unilateral papillary cystadenoma of the right epididymis (PCE). His past medical history is remarkable for Von Hippel–Lindau disease (VHLD), bilateral renal clear cell carcinoma, and hemangioblastomas. The patient noticed an abnormality with mild tenderness in the right scrotum. Ultrasound (US) of the right scrotum demonstrated a solid and cystic epididymal lesion. In this case report, we present the sonographic features of the PCE in the setting of a patient with VHLD.
Keywords
Papillary cystadenoma
Epididymis
Scrotal
Ultrasound
Testis
Von Hippel–Lindau disease
INTRODUCTION
Papillary cystadenoma of the epididymis (PCE) is a rare epithelial tumor that occurs sporadically or in association with Von Hippel–Lindau disease (VHLD).[1] It is the second most common benign neoplasm of the epididymis after the adenomatoid tumor.[2] PCE was first described in 1956, and since then has been recorded in approximately 70 reports that have been published as of 2014.[2,3] Bilateral PCE is pathognomonic of VHLD. In unilateral PCE, a review of 59 cases by Odrzywolski and Mukhopadhyay found that the association to VHL disease is about 29.3%, compared to the two-thirds of patients found to be positive for VHL disease with bilateral PCE.[2] Unilateral PCE is a rare but benign manifestation of VHLD, and once the lesion has been properly identified by imaging, the patients generally have a good prognosis after complete excision.[3] In this case, the patient presented with a unilateral PCE with an established diagnosis of VHLD and previous history of renal cell carcinoma (RCC). In this case report, we present the sonographic features of the PCE in the setting of a patient with VHLD.
CASE REPORT
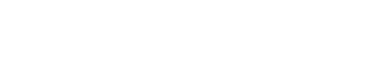
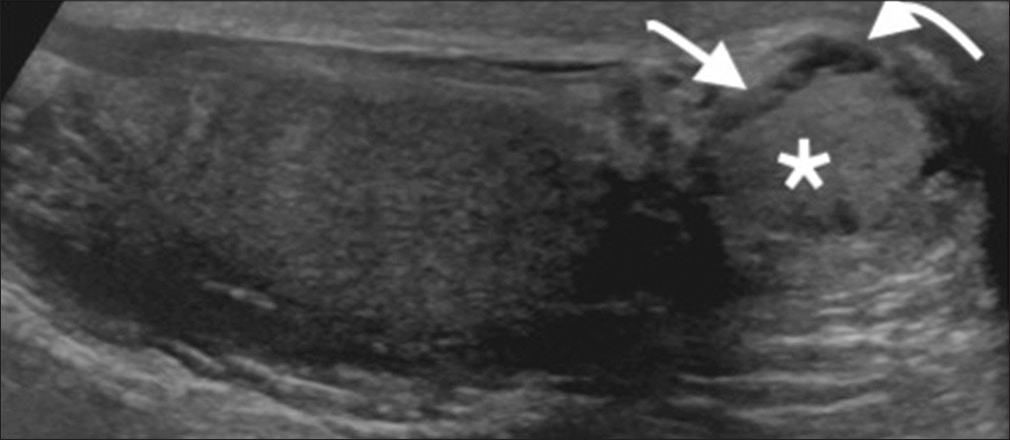
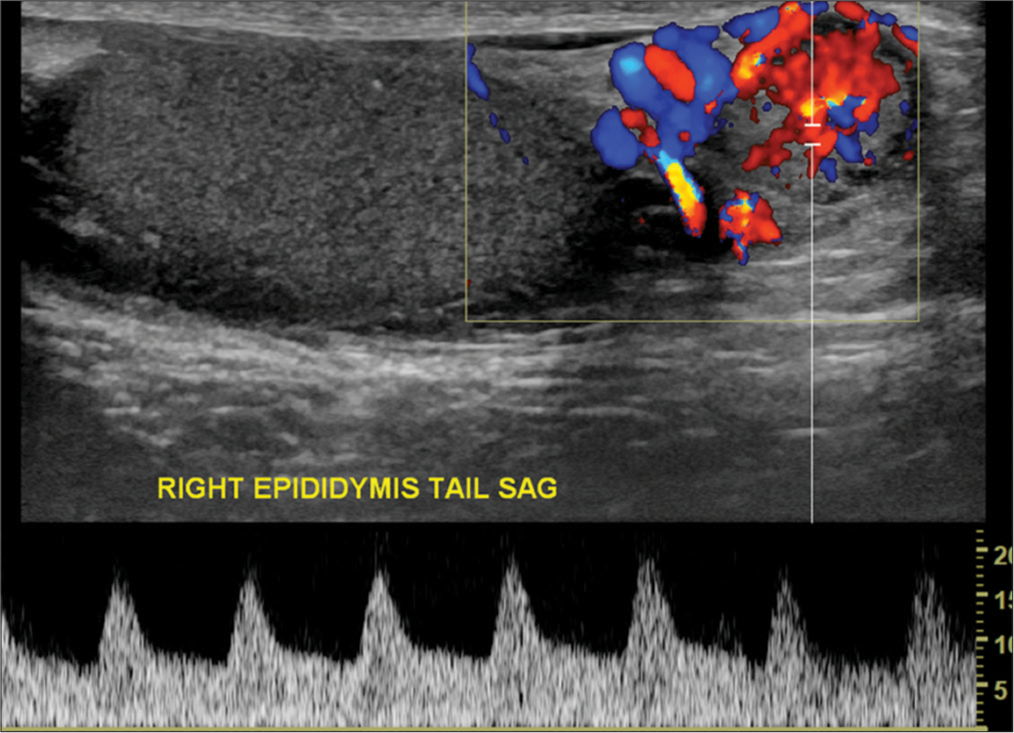
A 34-year-old male presented with a lump in his right scrotum of 1-week duration. The patient reported slight tenderness to touch but denied urinary tract symptoms such as increased frequency, dysuria, and voiding difficulty. No history of trauma, his past medical history is significant for VHLD, multiple hemangioblastomas of spine and brain, multiple bilateral renal masses, and renal clear cell carcinoma. His surgical history is remarkable for a left partial nephrectomy in 2013 for the removal of renal carcinoma. On physical examination, a 1 cm nodule was palpated over the right epididymis. The left testis and epididymis were unremarkable. There was no inguinal lymphadenopathy or inguinal hernia. The scrotal ultrasound (US) demonstrated a mixed cystic and solid lesion of the right epididymal tail measuring 1.2 cm with increased vascular flow (Figures 1 and 2). Scrotal examination did not reveal any other abnormality. A differential diagnosis of renal metastasis, adenomatoid tumor, and leiomyoma of the epididymis was advanced. Epididymitis was not considered because of the absence of any sexual history or urinary symptoms. The patient underwent orchiectomy, and it was confirmed to be a papillary cystadenoma on histopathology (Figure 3).
- A 34-year-old male with Von Hippel–Lindau disease presented with the right testicular tenderness and abnormality. Longitudinal gray-scale ultrasound of the right epididymis tail demonstrates a predominantly solid lesion (asterisk) with subtle peripheral cystic changes (curved arrow). In addition, a hypoechoic halo can be seen around the central solid lesion (straight arrow) confirmed to be papillary cystadenoma of the epididymis at surgery.
- A 34-year-old male with Von Hippel–Lindau disease presented with the right testicular tenderness and abnormality. Color flow and spectral Doppler of the right epididymis tail in sagittal plane demonstrates increased vascularity.
- A 34-year-old male with Von Hippel–Lindau disease presented with the right testicular tenderness and abnormality. Histopathology (Hematoxylin and Eosin stain, ×5) demonstrates papillary fronds covered with epithelial cells filled with clear cytoplasm projecting into cystic spaces (short arrow). Arrow shows normal epididymis.
DISCUSSION
This case report highlights the approach to a unilateral papillary cystadenoma of the epididymis (PCE) of the right epididymal tail. Both testes were normal, and the left epididymis was normal. Common tumors of epididymis include adenomatoid tumors, leiomyomas, fibromas, sperm granulomas, metastatic disease, and rarely papillary cystadenomas.
The most common cause of enlargement of the epididymal tail is epididymitis. Epididymitis is most commonly caused by Neisseria gonorrhoeae and Chlamydia trachomatis in younger men generally <35 years old.[4] US imaging of epididymitis reveals an enlarged and heterogeneous epididymis that is hypoechoic compared to the testis.[4] However, this history was not present in our patient. Therefore, epididymitis was not considered in the differential diagnosis. Other lesions that can present in the epididymal tail as solid masses include adenomatoid tumors, leiomyomas, and fibromas of the epididymis.
Adenomatoid tumors are benign and found in men with the majority being diagnosed in patients 20–50 years old.[4-6] These are the most common of the solid epididymal tumors with a prevalence of 73%.[6-8] Adenomatoid tumors may occur anywhere in the epididymis but occur most frequently in the tail.[4] The appearance on US scans vary greatly, but they typically appear hypoechoic, homogeneous, and with no significant vascularity.[4]
Leiomyoma of the epididymis is the second most common primary neoplasm of the epididymis at 11%.[7] When using US to image leiomyomas, these were found to have homogeneous echotexture, which is isoechoic or slightly hyperechoic to that of the testis.[7]
Fibromas of the epididymis often mimic neoplasms, but the lesions are more of a benign fibroinflammatory reaction resulting in nodules.[4,9] These lesions have been seen in patients 7–95 years old.[4] On US evaluation, the proliferation of fibrous and cellular tissue may appear as a well-defined hyperechoic or hypoechoic mass on US.[9]
Sperm granulomas can often be seen in up to 42% of men after vasectomy.[4] These granulomatous lesions form as a foreign body giant cell reaction to extravasated sperm.[4,10] US imaging shows generally well-defined, hypoechoic, and solid masses.[4] However, this patient has not had a vasectomy performed before his presenting symptoms.
Metastasis to the epididymis accounts for the secondary prevalence peak among men 71–90 years of age.[11] Testicular neoplasms are extremely rare and over 90% of testicular cancers arise from primary testicular lesions. However, the most common source of epididymal solid malignant neoplasms is metastasis.[10] The most frequent primary sources of metastasis to the testes is from the prostate (35%) and the lung (19%).[8,11,12] RCC can also metastasize to the epididymis in extremely rare cases.[13]
PCE may occur in people with VHLD either as a manifestation of VHLD or sporadically (60%).[2] PCE associated with VHLD tend to present bilaterally (almost pathognomonic for VHLD) and up to 40% of cystadenomas are bilateral.[4,14] These lesions are called papillary cystadenomas, but more often are found as small and compact solid lesions with cystic spaces commonly involving the epididymal head and not tail.[4] Appearances range from a primarily cystic mass (containing intramural solid components) to a mixed, but mostly solid mass (little or no cystic components) on US scans with increased vascularity.[4,14]
In our patient, in addition to solid and subtle cystic changes, there was a hypoechoic halo around the central solid lesion and cystic changes were present in the hypoechoic halo (Figure 1).
PCE is found mostly in young adults, although the patients can range in age from 16 to 76 years, with a mean age of 35 years.[15] More than one-third of the papillary cystadenoma cases reported in the literature are in patients with VHLD.[15] Therefore, an epididymal nodule found in a patient with VHLD is presumed to be a papillary cystadenoma.[15] However, when considering the differential diagnoses of epididymal tumors, metastatic RCC also cannot be excluded in patients with a history significant for RCC.[16] A definitive method of differentiating a benign PCE from RCC (both associated with VHLD) are histologic and immunohistochemical analysis. One-third of the patients with VHLD develop a PCE, while 24–45% of VHLD patients develop clear cell RCC.[2,15] Histologically, PCE resembles RCC, with cystic spaces and intracystic papillary projections lined by clear cells.[15] Immunohistochemically, PCE stains positively with soybean agglutinin, which is not observed in RCC.[1] Papillary cystadenomas also stain positively for CK7 and negatively for CD10, although in minor cases with only a focally reactive immunostain for CD10 in the stroma.[1,15-17] RCC staining profiles are typically negative for CK7 and immunoreactive for RCC and CD10.[1,16]
Our patient underwent orchiectomy and histopathology confirmed the diagnosis of PCE. Histopathology of papillary cystadenomas has a distinctive look, with prominent papillae lined by glycogen-rich clear cells (Figure 3).[4]
VHLD is a multisystem genetic disorder caused by germline mutation in the VHL tumor suppressor gene that is an autosomal dominant disorder.[18-20] VHLD manifests as retinal and central nervous system hemangioblastomas involving the posterior fossa, clear cell RCC, rhabdomyomas involving the heart, pheochromocytomas involving the adrenal gland, pancreatic islet tumors, endolymphatic sac tumors, and epididymal cystadenomas.[18,20] The two clinical types of VHLD exist and are based on the presence or absence of pheochromocytoma.[19] VHL Type 1 is associated with a lower risk of developing pheochromocytomas.[19] VHL Type 2 is associated with high risk for developing pheochromocytoma.[19] VHL Type 2 is then subdivided into Type 2A and 2B, associated with a lower and higher risk for RCC.[19]
All renal cysts in patients with VHLD are presumed to be carcinomas because cysts may change to form tumors.[20] Renal cysts occur in 59–69% and RCC occurs in 24–45% of patients with VHLD, with metastatic RCC being the leading cause of death for one-third of VHLD patients.[20,21]
High-frequency US and color flow Doppler are the first modalities of choice for the evaluation of epididymal and testicular lesions.[4,8-10,22,23] This allows the examiner to distinguish benign from malignant lesions as well as identify intratesticular from extratesticular pathologic conditions.[4,23-25] Malignant masses characteristically include larger diameters, volume, and increased vascularity.[10] US imaging is the preferred modality for imaging palpable testicular lesions, especially for children younger than 16 years, to avoid exposure to radiation or contrast media.[24,26] On the other hand, computed tomography (CT) is more useful as the standard for cancer staging.[23] In addition, contrast-enhanced CT of the abdomen and pelvis can be performed in patients suspected of having VHLD to screen for visceral manifestations of the disease.[26] Radiographic screening of asymptomatic patients at high risk for VHLD or for patients with established diagnoses may enhance both the length and the quality of life of patients.[26]
CONCLUSION
PCE presenting as a unilateral epididymal mass necessitates further investigation. This is especially true for patients with a medical history significant for VHLD and RCC because the possibility of metastatic RCC must be eliminated. However, they do occur in patients that do not have VHLD. Although there are imaging and histological similarities between PCE and RCC, CK7 and CD10 are reliable immunohistochemical markers to distinguish the two.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Vikram Dogra is on the Editorial Board of the Journal.
References
- Clear cell papillary cystadenoma of epididymis, a mimic of metastatic renal cell carcinoma. J Pak Med Assoc. 2008;58:209-11.
- [Google Scholar]
- Papillary cystadenoma of epididymis: Is there a need for further investigation in unilateral cases? Int J Surg Case Rep. 2013;4:616-8.
- [CrossRef] [PubMed] [Google Scholar]
- Solid variant of papillary cystadenoma of the epididymis. Histopathology. 2015;67:138-41.
- [CrossRef] [PubMed] [Google Scholar]
- From the archives of the AFIP: Extratesticular scrotal masses: Radiologic-pathologic correlation. Radiographics. 2003;23:215-40.
- [CrossRef] [PubMed] [Google Scholar]
- Adenomatoid tumors of the testis: A report of two cases and review of the literature. Oncol Lett. 2014;7:1718-20.
- [CrossRef] [PubMed] [Google Scholar]
- Adenomatoid tumor of epididymidis: A case report. Cases J. 2008;1:206.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyoma of the epididymis treated with partial epididymectomy. Urol Ann. 2014;6:356-58.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of non-neoplastic intratesticular masses. Diagn Interv Radiol. 2011;17:52-63.
- [Google Scholar]
- Benign and malignant epididymal masses evaluated with scrotal sonography: Clinical and pathologic review of 85 patients. J Ultrasound Med. 2008;27:1195-202.
- [CrossRef] [PubMed] [Google Scholar]
- From the archives of the AFIP: Tumors and tumorlike lesions of the testis: Radiologic-pathologic correlation. Radiographics. 2002;22:189-216.
- [CrossRef] [PubMed] [Google Scholar]
- Testicular metastasis in a case of squamous cell carcinoma of the lung. Case Rep Oncol. 2015;8:133-7.
- [CrossRef] [PubMed] [Google Scholar]
- Renal cell carcinoma metastases to the spermatic cord: review of the literature and case presentation. J Clin Oncol. 2013;6:427-31.
- [CrossRef] [Google Scholar]
- Clear cell papillary cystadenoma with sonographic and histopathologic correlation. J Ultrasound Med. 2006;25:1451-3.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary cystadenoma of the epididymis associated with von hippel-lindau disease diagnosed on fine needle aspiration cytology. Cytopathology. 2014;25:279-81.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary cystadenofibroma of epididymis: A case report. Int J Clin Exp Pathol. 2011;4:629-31.
- [Google Scholar]
- von hippel-Lindau disease: A clinical and scientific review. Eur J Hum Genet. 2011;19:617-23.
- [CrossRef] [PubMed] [Google Scholar]
- Expression of vascular endothelial growth factor in von hippel-lindau syndrome-associated papillary cystadenoma of the epididymis. Hum Pathol. 1998;29:1322-4.
- [CrossRef] [Google Scholar]
- Renal cystic diseases and renal neoplasms: A mini-review. Clin J Am Soc Nephrol. 2009;4:1998-2007.
- [CrossRef] [PubMed] [Google Scholar]
- Incidentally detected non-palpable testicular tumours in adults at scrotal ultrasound: Impact of radiological findings on management radiologic review and recommendations of the ESUR scrotal imaging subcommittee. Eur Radiol. 2016;26:2268-78.
- [CrossRef] [PubMed] [Google Scholar]
- Testicular cancer: What the radiologist needs to know. AJR Am J Roentgenol. 2013;200:1215-25.
- [CrossRef] [PubMed] [Google Scholar]
- Benign intratesticular cystic lesions: US features. Radiographics. 2001;21:S273-81.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of ultrasound-guided testicle sparing surgery for small testicular masses. J Ultrasound. 2016;19:29-33.
- [CrossRef] [PubMed] [Google Scholar]
- Von hippel-lindau disease: Radiologic screening for visceral manifestations. Radiology. 1990;174:815-20.
- [CrossRef] [PubMed] [Google Scholar]