Translate this page into:
Rare Cause of Painful Ejaculation – Zinner’s Syndrome: A Case Report

*Corresponding author: Suriyaprakash Nagarajan, Department of Radiodiagnosis, Government Kilpauk Medical College Hospital, Chennai, Tamil Nadu, India. cbesuriya@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jaganathan D, Kathirvelu G, Nagarajan S, Ganesan UN. Rare Cause of Painful Ejaculation – Zinner’s Syndrome: A Case Report. Am J Sonogr 2020;3:1.
Abstract
Zinner’s syndrome is a rare congenital abnormality consisting of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ipsilateral ejaculatory duct obstruction. The mutual embryological origins of the seminal vesicle and the ureteral bud from the Wolffian duct result in both anomalous seminal vesicle and urinary tracts. Most cases have nonspecific symptoms such as prostatism, urinary urgency, dysuria, painful ejaculation, and perineal discomfort. The usual presentation is between the third and fourth decades of life, with infertility being the most common complaint. Ultrasound and magnetic resonance imaging can easily detect this condition. We present here an extremely rare developmental anomaly involving the Wolffian ducts, which would remain undiagnosed but for radiologic imaging.
Keywords
Magnetic resonance imaging
Painful ejaculation
Seminal vesicle cyst
TRUS
Zinner’s syndrome
INTRODUCTION
Congenital malformations of the seminal vesicles are very uncommon. Congenital abnormalities involving the urogenital system ranging from innocuous condition such as duplication of the ureter to life-threatening condition such as bilateral renal agenesis. Maldevelopment of the distal Wolffian duct causes absence of the ureteral bud with seminal vesicle cystic malformation.[1] Zinner’s syndrome is a rare congenital abnormality consisting of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ipsilateral ejaculatory duct obstruction.[2] Ever since 1914, when Zinner described the syndrome, <200 cases of seminal vesicle cysts associated with ipsilateral renal agenesis have been reported in the literature.[3]
CASE REPORT
A 28-year-old adult male presented with pain during ejaculation and dysuria for 3 years. He also complained of decreased quantity of semen during ejaculation. There was a history of infertility as he had been married for 3 years and his spouse had not conceived. The patient had no endocrine or systemic disease. The physical examination revealed normally developed external genitalia. His surgical history was not significant. The routine blood and urine analysis workup and biochemical tests were normal. Semen examination was done, and the sperm count was reported to be 40 million with a semen volume of 1 mL (normal reference range of sperm count is >20 million sperms and 2–6 mL ejaculate volume).
Investigation and management
The patient was sent to our department for further evaluation. Ultrasonogram [Figure 1] of abdomen showed the absence of kidney in the left renal fossa and a cystic mass in the left side of pelvis in the region of seminal vesicle.
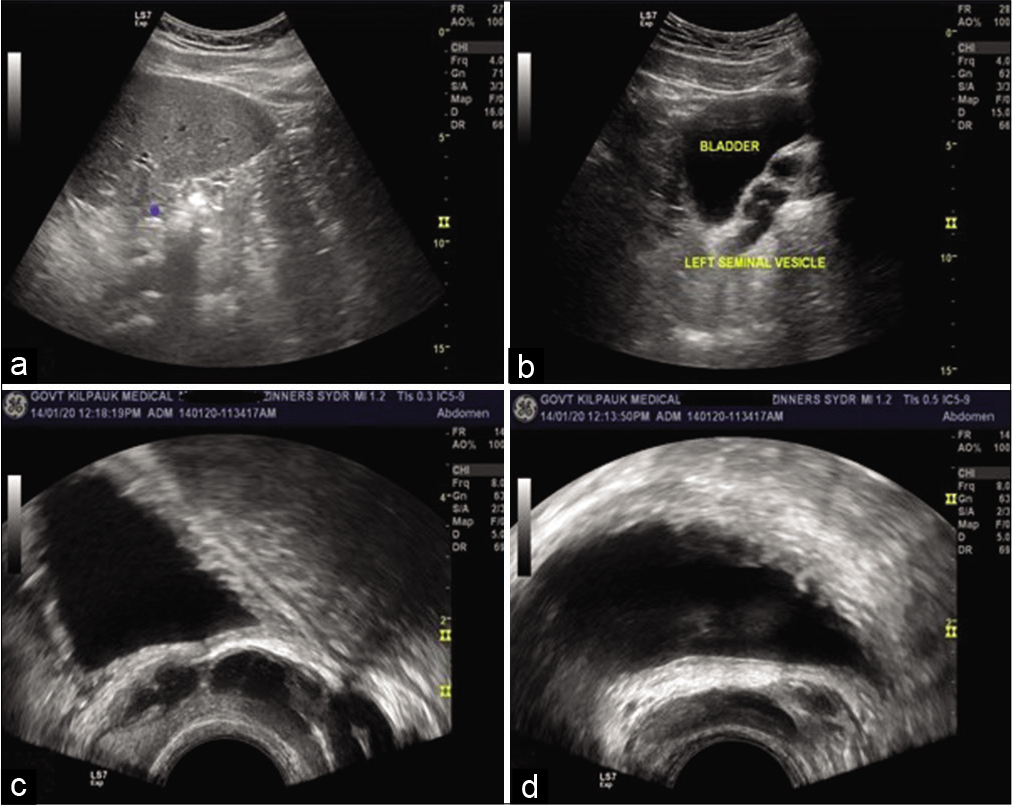
- A 28-year-old adult male presented with pain during ejaculation and primary infertility. (a) Transabdominal ultrasound (USG) in the left hypochondriac region shows absent kidney in the left renal fossa. (b) Pelvic ultrasonography shows cystic tubular structure posterior and to the left of the urinary bladder extending up to the midline. (c) Transrectal USG shows cystic appearing left seminal vesicle. (d) TRUS showing normal appearing right seminal vesicle.
MR demonstrated multiple cystic-to-tubular structures in the left seminal vesicle [Figure 2a-c] appearing hyperintense on both T2-weighted and T1W images. Right seminal vesicle appears normal [Figure 2c]. The absent left kidney [Figure 2d] was confirmed on coronal MR images. A dilated tortuous tubular structure was seen coursing along the left iliac vessels toward the midline terminating in the left seminal vesicle. It had no connection with the bladder. It was diagnosed to be an ectopic atretic ureter [Figure 3].
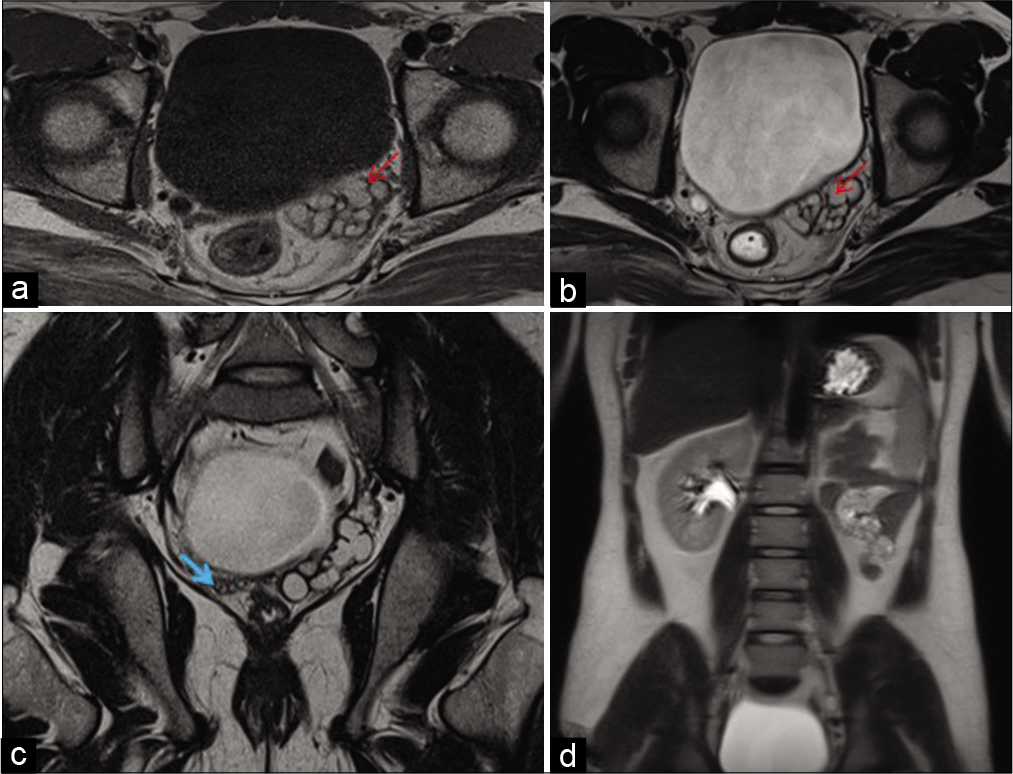
- A 28-year-old adult male presented with pain during ejaculation and primary infertility. (a and b) Axial T1 and T2 TSE sequences show multiple cystic hyperintense structures lying close together, in the region of the left seminal vesicle (red arrow). (c) Coronal T2WI images normal right seminal vesicle (blue arrow) – left seminal vesicle cyst. (d) Coronal T2-weighted HASTE MRI showing normal right kidney and absence of the left kidney – left renal agenesis.
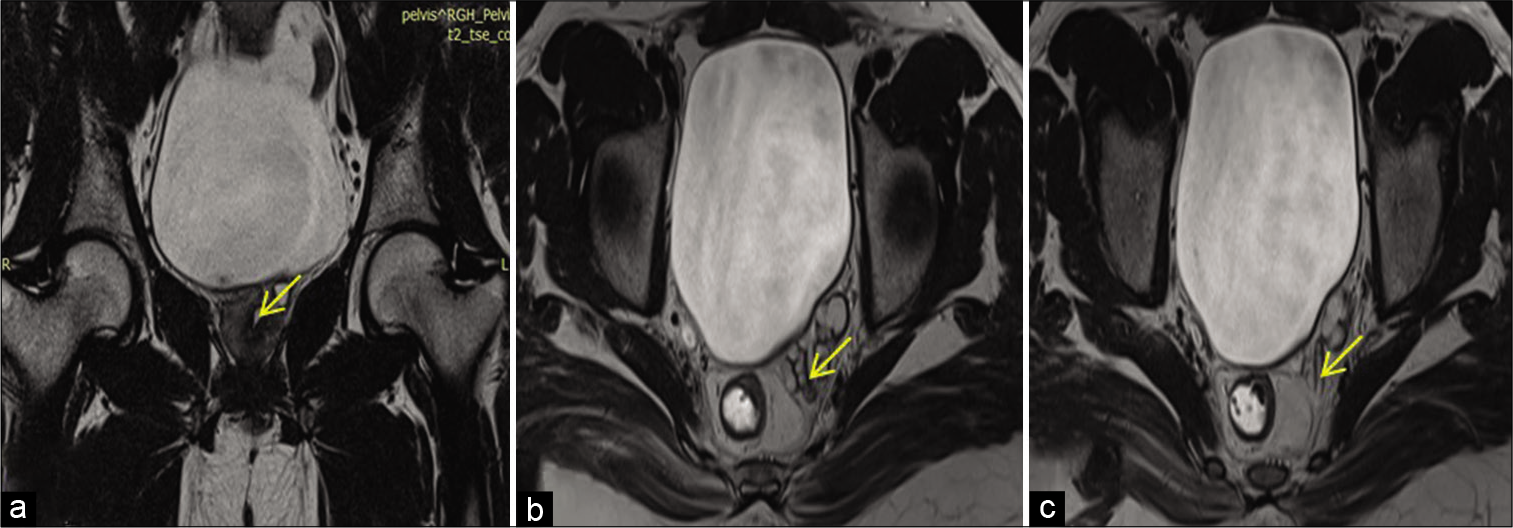
- A 28-year-old adult male presented with pain during ejaculation and primary infertility. (a) Coronal T2WI showing obstruction of ejaculatory duct (yellow arrow). (b and c) Consecutive axial T2-weighted TSE MRI showing dilated tortuous vas deferens (yellow arrow) – left ejaculatory duct obstruction.
MR findings of grossly dilated left ejaculatory duct [Figure 4] with seminal vesicle cysts, along with the visualization of atretic left ureter and left renal agenesis lead to the diagnosis of Zinner’s syndrome, which is a developmental anomaly of the Wolffian duct.
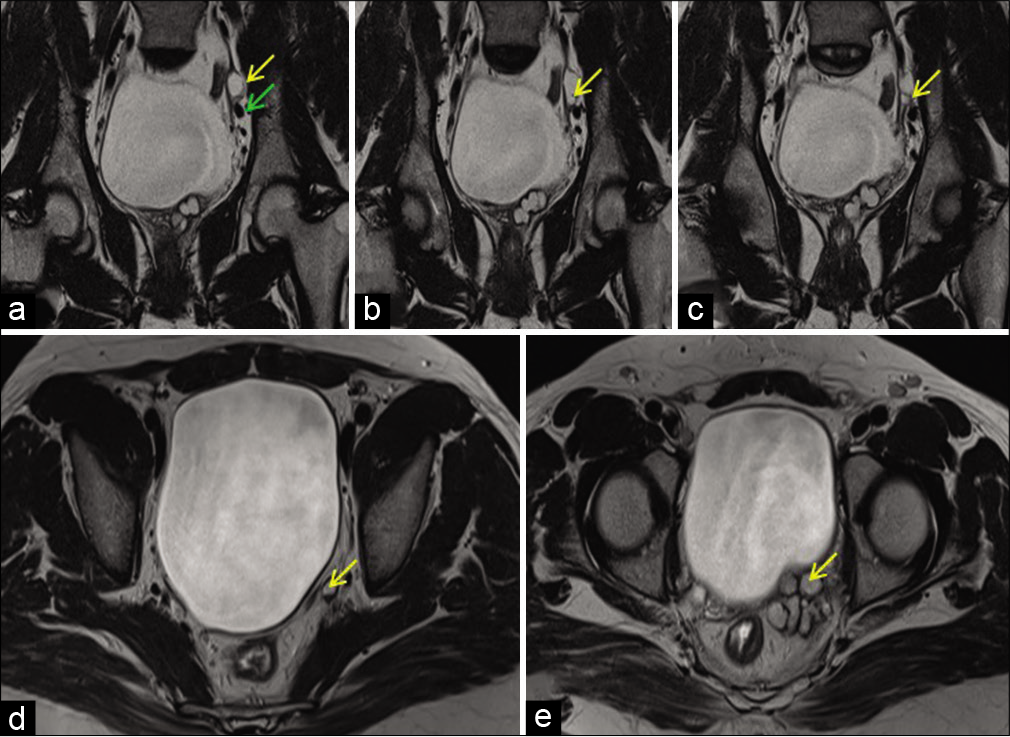
- A 28-year-old adult male presented with pain during ejaculation and primary infertility. (a-c) Consecutive coronal T2WI showing hyperintense dilated tubular structure(yellow arrow) in pelvis adjacent to iliac vessels (green arrow). (d and e) Consecutive axial T2-weighted TSE MRI showing hyperintense left remnant ureter (yellow arrow) draining into an ipsilateral seminal vesicle cyst – atretic left ureter.
DISCUSSION
Zinner’s syndrome is a triad of Wolffian duct anomaly comprising of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ejaculatory duct obstruction.[4] Maldevelopment of Wolffian duct occurs before the 7th week when the ureteric bud forms from the distal portion. The seminal vesicle originates from Wolffian duct under the effect of testosterone. Hence, maldevelopment of Wolffian duct results in cystic seminal vesicle and ipsilateral renal agenesis.[5]
Patients with Zinner’s syndrome are usually symptomatic in the 2nd–4th decade of their life and common chief complaints will be genitourinary symptoms, including irritative and obstructive lower urinary tract symptoms, perineal pain, painful ejaculation, infertility, and hematospermia.[5] Symptoms are due to progressive dilation of seminal vesicles due to accumulation of secretions following insufficient drainage secondary to ejaculatory duct obstruction.[5] The seminal vesicles are situated directly posterior to bladder, and therefore, enlarged cysts can cause bladder irritation leading to symptoms of dysuria, recurrent urinary tract infections, infertility, painful ejaculation, epididymitis, and prostatitis.[6] Ejaculatory duct obstruction leads to the characteristic symptoms of dysuria and causes infertility in this rare developmental anomaly of the male genitor-urinary system.[2]
Painful ejaculation is also known as dysorgasmia or orgasmalgia. Most common causes of painful ejaculation include prostatitis, urethral calculus, ejaculatory duct obstruction, pudendal neuropathy, and radiation. Certain antidepressant medications may also lead to painful ejaculation. Imaging may be helpful only in select cases of painful ejaculation. Zinner’s syndrome can cause painful ejaculation due to ejaculatory duct obstruction.
USG is a good imaging modality in diagnosing this condition as it is highly accurate, easily available and has no risk of radiation.[7] In USG, dilated and cystic seminal vesicle can be mistaken for an ectopic, retrovesical, and severely hydronephrotic kidney. This underlies the importance of other modalities when in doubt.
Ultrasonography is cheap, easily available, quick and has no radiation risk
Computed tomography and magnetic resonance imaging (MRI) can demonstrate the cysts with superior soft-tissue resolution. MRI as a radiation free modality is superior to CT for delineating the genitourinary anomalies and demonstrating peripheral pelvic structure for surgical plan decision. Simple seminal vesicle cysts without associated renal agenesis are due to expansion of the seminal vesicle tubes and are round or ovoid with regular margins. Seminal vesicle cysts of Zinner’s syndrome derived from the remaining Wolffian duct are usually larger, round, or tubulosaccular with irregular margins.[8] Seminal vesicle cysts have varying signal intensity on T1WI and fluid signal intensity on T2WI. Increased T1-weighted intensity reflects hemorrhage or increased concentration of proteinaceous fluid. Differential diagnosis of seminal vesicles cysts includes prostatic utricle cyst, ureteroceles, Müllerian duct cysts, and ejaculatory duct cysts. Tubulosaccular or a large rounded cystic lesion in seminal vesicle region with ipsilateral renal agenesis provides the clue to diagnose Zinner’s syndrome. Atresia of the ejaculatory duct is due to the developmental abnormality of the distal part of Wolffian ducts.[9] MRI can show the connection between ectopic ureter and seminal vesicle.
Treatment is usually indicated in symptomatic patient. Treatment options range from medical treatment, percutaneous drainage, transurethral aspiration and alcohol injection, transrectal aspiration, laparoscopy, and even open cyst surgery.
Imaging helps in definitive diagnosis and is also useful for surgical planning of seminal vesicles cyst excision, as it shows anatomic relationships between the different pelvic structures.
CONCLUSION
Developmental anomalies of the urogenital system are not considered by clinicians when patients present with vague symptoms and hence imaging alone has the ability to provide an accurate diagnosis. Sonography is the first imaging modality in evaluation and diagnosis of Zinner’s syndrome and it helps in accurate diagnosis in most of the cases. MRI is the best imaging modality for diagnosing genital tract developmental anomalies in both males and females as the anatomic delineation is precise. Imaging is definite for confirming the triad of findings associated in Zinner’s syndrome.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Imaging findings of congenital anomalies of seminal vesicles. Pol J Radiol. 2019;84:25-31.
- [CrossRef] [PubMed] [Google Scholar]
- Zinner syndrome a rare developmental anomaly of the mesonephric duct diagnosed on magnetic resonance imaging. Radiol Case Rep. 2016;11:313-7.
- [CrossRef] [PubMed] [Google Scholar]
- Zinner's syndrome: Report of two cases and review of the literature. Basic Clin Androl. 2016;26:10.
- [CrossRef] [PubMed] [Google Scholar]
- Zinner syndrome: A unique triad of mesonephric duct abnormalities as an unusual cause of urinary symptoms in late adolescence. Indian J Urol. 2010;26:444-7.
- [CrossRef] [PubMed] [Google Scholar]
- Management of zinner's syndrome associated with contralateral seminal vesicle hypoplasia: A case report. Case Rep Urol. 2013;2013:1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Zinner syndrome: An unusual cause of bladder outflow obstruction. BJR Case Rep. 2017;3:20160094.
- [CrossRef] [PubMed] [Google Scholar]
- Unique association of multiple seminal vesicle cysts with contralateral renal agenesis: A rare variant of zinner syndrome. Cureus. 2017;9:e1415.
- [CrossRef] [Google Scholar]
- Zinner's syndrome: Clinical features and imaging diagnosis. Asian J Androl. 2018;20:316-7.
- [CrossRef] [PubMed] [Google Scholar]
- Zinner syndrome diagnosed by magnetic resonance imaging and computed tomography: Role of imaging to identify and evaluate the uncommon variation in development of the male genital tract. Radiol Case Rep. 2017;12:54-8.
- [CrossRef] [PubMed] [Google Scholar]







